Blog
-
Medicaid Unwinding Will Begin in April but There’s Good News in Congressional Funding Agreement
[Editor’s Note: The bipartisan spending plan was approved by Congress and signed into law by the President on December 29, 2022. Read CCF’s brief to learn more.] Congress has just reached an end of the year funding agreement, and it has very significant implications for the more than 90 million people who rely on Medicaid…
-
Congress Includes Medicaid, CHIP Mental Health Provisions in End of Year Funding Bill
[The bipartisan spending plan was approved by Congress and signed into law by the President on December 29, 2022. Read CCF’s brief to learn more.] As my colleagues on Say Ahhh! have highlighted the omnibus appropriations bill released earlier today includes a number of provisions related to Medicaid and CHIP such as funding for Puerto…
-
End of the Year Appropriations Bill Would Avert Medicaid Fiscal Cliff for Puerto Rico and the Territories
[Editor’s Note: The bipartisan spending plan was approved by Congress and signed into law by the President on December 29, 2022. Read CCF’s brief to learn more.] The bipartisan omnibus appropriations bill, which was unveiled early this morning by the Senate Appropriations Committee, would avert the dire Medicaid fiscal cliff facing Puerto Rico and the…
-
Medicaid Managed Care in 2022: The Year that Was
2022 was another year of growth in Medicaid managed care. Growth in enrollment. Growth in spending. There was even a modest—but most welcome—growth in transparency about the performance of Medicaid managed care organizations (MCOs) from 2021. Here are some of the top-line developments at the national and state level. The MCO Industry As of March…
-
New Report Underscores Need to Reassure Immigrant Families
Researchers from the Urban Institute have documented the chilling effects of the Trump-era public charge regulation and other anti-immigrant policies for the past several years. Unfortunately, new research confirms that families are continuing to avoid public programs due to immigration-related concerns, despite having material hardships such as food insecurity, unmet medical needs, and problems paying…
-
Early Research Shows Benefits of One Year of Postpartum Medicaid
Over the last several months, we’ve seen the Biden Administration approve more than half of states to extend postpartum Medicaid coverage for one year after the end of pregnancy. Congress too has also considered proposals to require all states to offer 12 months of postpartum Medicaid coverage, which many advocates continue to champion to ensure…
-
Medicaid Managed Care: Quality Performance, Sanctions, and Transparency in California
Three years ago, the California Health Care Foundation published a ground-breaking report on Medicaid managed care in the state. Researchers from the University of California at San Francisco presented and analyzed data on the quality of care furnished by each Medicaid managed care organization (MCO) over the 10-year period 2009 – 2018. The researchers found that, over…
-
Unwinding Wednesday #14: More States Make Unwinding-Related Materials Publicly Available
Just over three months ago, we published our 50-State Unwinding Tracker, kicking off our Unwinding Wednesday blog series. As we approach the end of the year, I want to reflect on the progress we’ve seen in our tracker of states publishing information and taking steps toward preparing for the unwinding. In our tracker, we identified…
-
Maternal Health Policies: Will Congress Act During the Lame Duck Session?
By Maggie Clark and Kay Johnson As the 117th Congress completes its work in the ”lame duck” session this month, policy makers are considering a range of maternal health policy priorities. These changes are urgently needed: the nation’s maternal mortality rate increased for the fourth year in a row in 2021, and the latest data…
-
Lesson from Pandemic: Medicaid Continuous Coverage Works!
New report on child health coverage shows improvement in child health coverage, reversing a negative trend prior to pandemic This year’s annual report on child health coverage is out after a hiatus last year due to the lack of available Census data. We’re happy to report some good news. The rate of uninsured children declined from…
-
Unwinding Wednesday #13: New Unwinding Resources, Including State-Specific Renewal Flyers
We are pleased to share new content on our unwinding resource page. State-Specific Renewal Flyers We are particularly pleased to announce the addition of state-specific renewal flyers that include the state agency website and toll-free numbers. One set of flyers also includes the income eligibility levels for children and adults, the other does not. The…
-
Mapping the Barriers to Renewing Medicaid Coverage for Rural Arizonans When Continuous Coverage Ends
By Zaida Dedolph Piecoro and Bryna Koch Currently, half of those at risk of coverage loss at the end of the public health emergency (PHE) in Arizona are children under 19. Like many others, we at Children’s Action Alliance and our partners at the University of Arizona, Arizona Center for Rural Health are strategizing to…
-
Unwinding Wednesday #12: More States Are Taking Advantage of Flexibilities Aimed at Mitigating Gaps in Coverage during Unwinding
A few months ago, we wrote about new data from CMS on approvals of time-limited waivers, or (e)(14) waivers, that states may adopt to smooth the unwinding process and mitigate unnecessary gaps in coverage. Only 20 states had been approved for these temporary waivers at the time the data was initially released. Since then, the…
-
States Can Help Address the Child Care Crisis by Prioritizing Health Coverage
Federal and state lawmakers are seeking policy solutions to address the child care crisis that was exacerbated by the pandemic. Workforce challenges loom large, with necessary attention to boost wages for the child care professionals who play a role in not only helping parents work, but also promoting early childhood development. But states can also…
-
New Report Highlights Role Medicaid Can Play in Advancing Comprehensive School Mental Health Services
Last month, the Healthy Schools Campaign and Mental Health America released a new report titled, “State Policy Opportunities: Advancing Comprehensive School Mental Health Systems to Support Students”, which provides a new perspective on the key actors that can play a role in advancing comprehensive school mental health systems for students. But what counts as a…
-
Federal Focus on Behavioral Health Crisis Care
You may be thinking that we’ve been writing a lot about behavioral health on Say Ahhh! lately. Well, you’re right – and there’s more! For starters, last week, the Substance Abuse and Mental Health Services Administration (SAMHSA) released new National Guidelines for Child and Youth Behavioral Health Crisis Care, complementing other recent resources such as…
-
Are Medicaid Enrollees Aware that Medicaid Renewals Will Restart Soon?
A new brief by the Urban Institute indicates that nearly two-thirds of adults (62 percent) who are covered by or have a Medicaid-enrolled family member are unaware that Medicaid renewals will be restarting in the future. Of those who had heard at least a little about the resumption of renewals, the largest source of information…
-
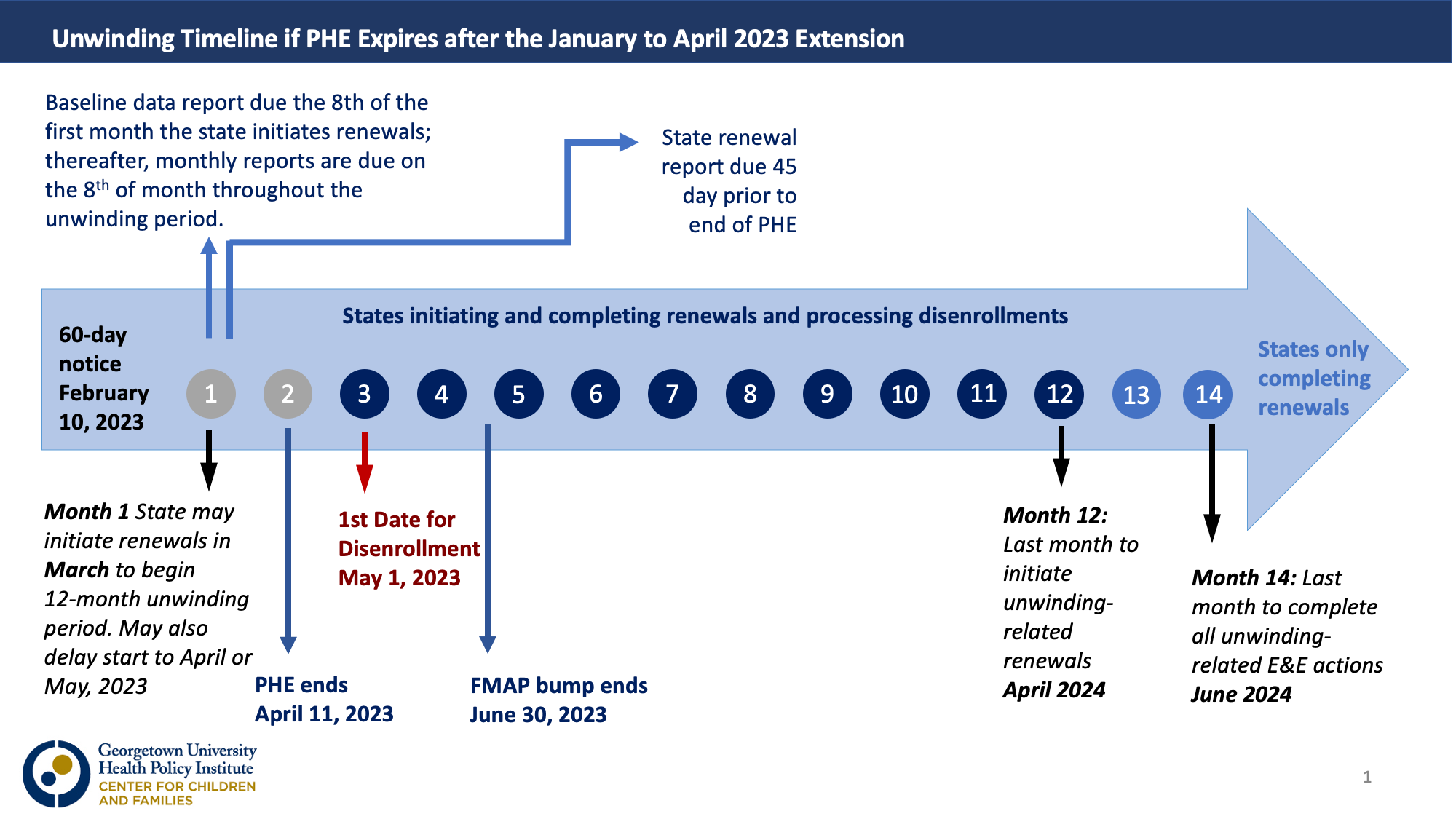
Unwinding Wednesday #11: No 60-day Notice on the Unwinding; PHE Expected to Be Extended Until April 2023
[Editor’s Note: The end-of-year bipartisan funding agreement released on December 20 would delink the continuous coverage requirement from the HHS Secretary’s declaration of a public health emergency and start the Medicaid “unwinding” process on April 1. The agreement includes 12 months of continuous coverage for children and other provisions designed to protect individuals eligible for…
-
States Leading the Way on Connecting All Children with Health Coverage – Will Congress Follow?
According to the Urban Institute, over half of the remaining uninsured children are eligible for Medicaid or the Children’s Health Insurance Program (CHIP) but unenrolled. About a third of uninsured children are ineligible for Medicaid or CHIP because their family income exceeds the eligibility thresholds. Another 10% are ineligible for Medicaid/CHIP because of their immigration…
-
Transparency in Medicaid Managed Care: The Power of the California Procurement Database
The Illinois Answers Project has just published a must-read piece of investigative reporting: “Insurance Giant Failed Foster Kids with Inadequate Care.” It raises a number of disturbing questions about the way children in foster care are being treated in the state’s Medicaid managed care program. About the performance of a Centene subsidiary that has contracted…