Medicaid
-
Proposed Changes to Medicaid Threaten Access to Health Care
In the 1990s, the Medicaid program was often discussed by policymakers as a secondary topic after dealing with issues surrounding Medicare and reforming managed care. There were several reasons for this. Medicaid was seen as a “welfare” program targeted at specific poor populations. The country still hadn’t yet experienced the deep recessions that would mean…
-
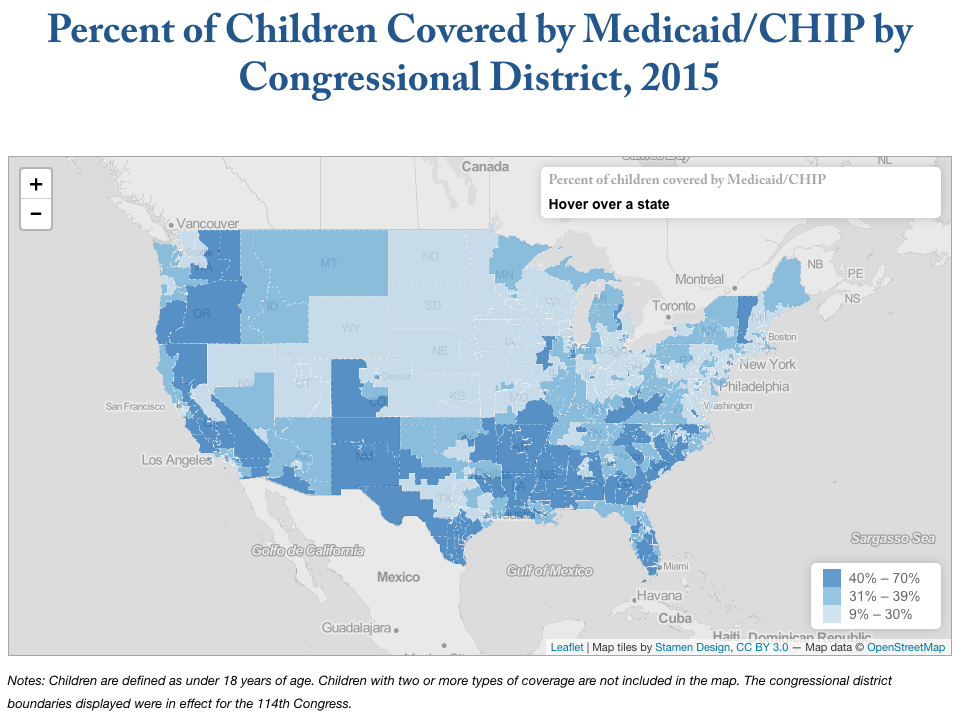
Medicaid’s Special Importance for Children in Southern and Western States
We can’t say it enough here at Georgetown CCF – Medicaid is critical for delivering quality health care to children and their families. Our state, county and congressional district maps make clear just how important Medicaid is to children across the country, regardless of which elected officials represent them in Washington, D.C. Nationally, children make…
-
The Passage of the AHCA: The Real Life Consequences for People with Disabilities
By Julie Ward, Director of Health Policy and Nicole Jorwic, Director of Rights Policy. This post originally appeared on The Arc Blog. They say that if you want to know about a person, look at how they spend their money; to know the values of a nation, the same is true. The current Affordable Care…
-
-
Senator Cassidy Tells Jimmy Kimmel He Wants to Protect Kids’ Health but Misses Point on Need to Preserve Medicaid to Achieve Goal
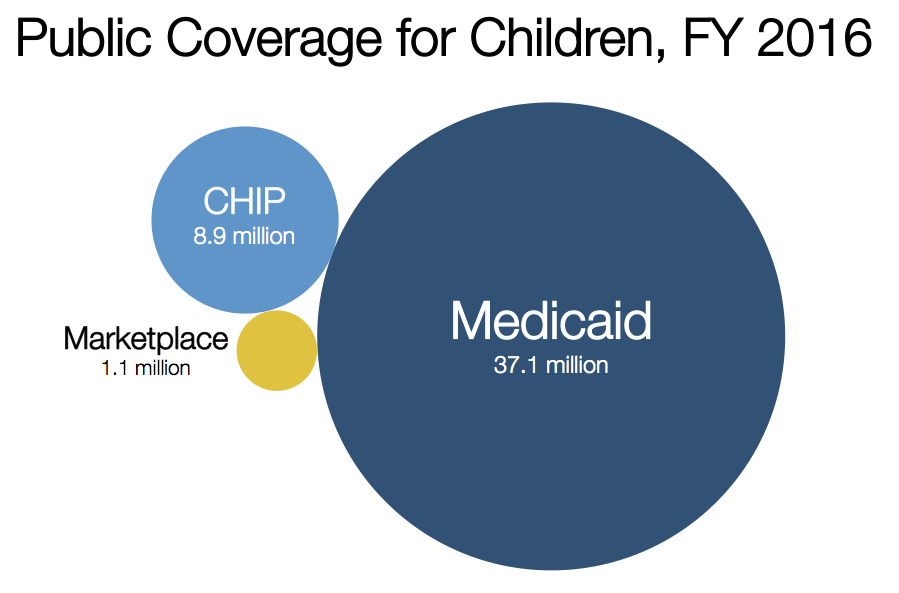
One of the largest challenges in showing the potential impact of the latest House-passed proposal to repeal the ACA is elevating the fact that our nation’s success in covering children is at major risk. Medicaid, accompanied by the Children’s Health Insurance Program (CHIP) and the Affordable Care Act (ACA), has been the primary reason our…
-
Capping Federal Medicaid Payments to States: Four Questions to Consider
Late last week, the House of Representatives, with one vote to spare, passed a bill to “repeal and replace” the Affordable Care Act (ACA). Among many other things, the bill would radically restructure the nation’s largest health insurer for children—Medicaid—by capping federal matching payments to states starting in three years and continuing each year after…
-
Nation’s Progress on Children’s Health Coverage Imperiled
On November 9th I blogged about what the election results could mean for child and family coverage. As readers of Say Ahhh! know, the nation made extraordinary progress in reducing the rate of uninsured children to under 5%, This progress is thanks to Medicaid, the Children’s Health Insurance Program (CHIP), and the Affordable Care Act (ACA). All three…
-
Five Myths about the Medicaid Cap
The White House and the House Leadership are hoping to bring a bill to “repeal and replace” the Affordable Care Act (ACA) to the House floor for a vote this week. The bill contains a new section allowing states to waive ACA consumer protections relating to health insurance. It also contains the same cap on…
-
Making Kids Wait for Coverage Makes No Sense in a Reformed Health System
A central goal of the Affordable Care Act (ACA) is near universal access to affordable health insurance through Medicaid, the Children’s Health Insurance Program (CHIP), and subsidies to help purchase private coverage in the new Health Insurance Marketplaces. As states full implement the ACA, they are modernizing the way Medicaid and CHIP do business, including…
-
Medicaid: Welcoming Americans with Pre-existing Conditions since 1965
The White House and the Republican Leadership in the House are continuing to look for enough votes to pass a bill to “repeal and replace” the Affordable Care Act (ACA). A number of Republican Members opposed to the bill have expressed specific concern about new amendment that would allow states to undo the ACA’s protections…
-
First Steps: A Spotlight on Health and Developmental Screenings for Young Texans
By Adriana Kohler and Rebecca Hornbach, Texans Care for Children Every family looks forward to their child’s first smile, first step, and first words. Routine well-child visits and developmental screenings allow doctors and families to monitor a child’s health and development and celebrate these kinds of milestones. Ongoing screenings for young children also help identify…
-
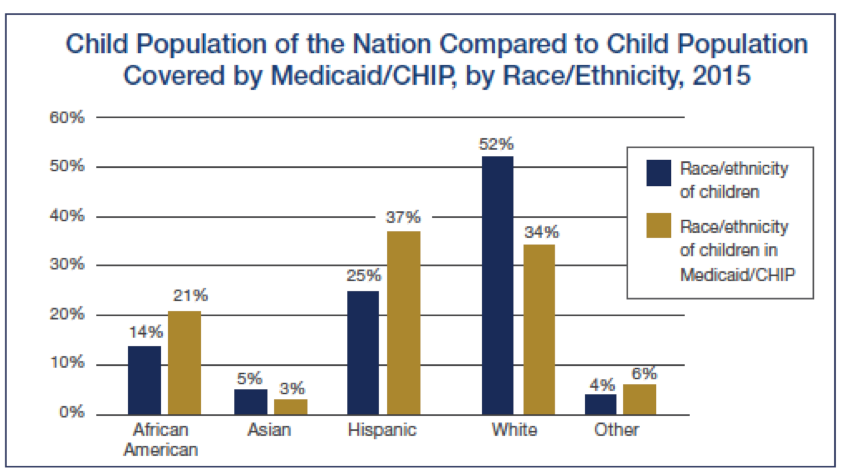
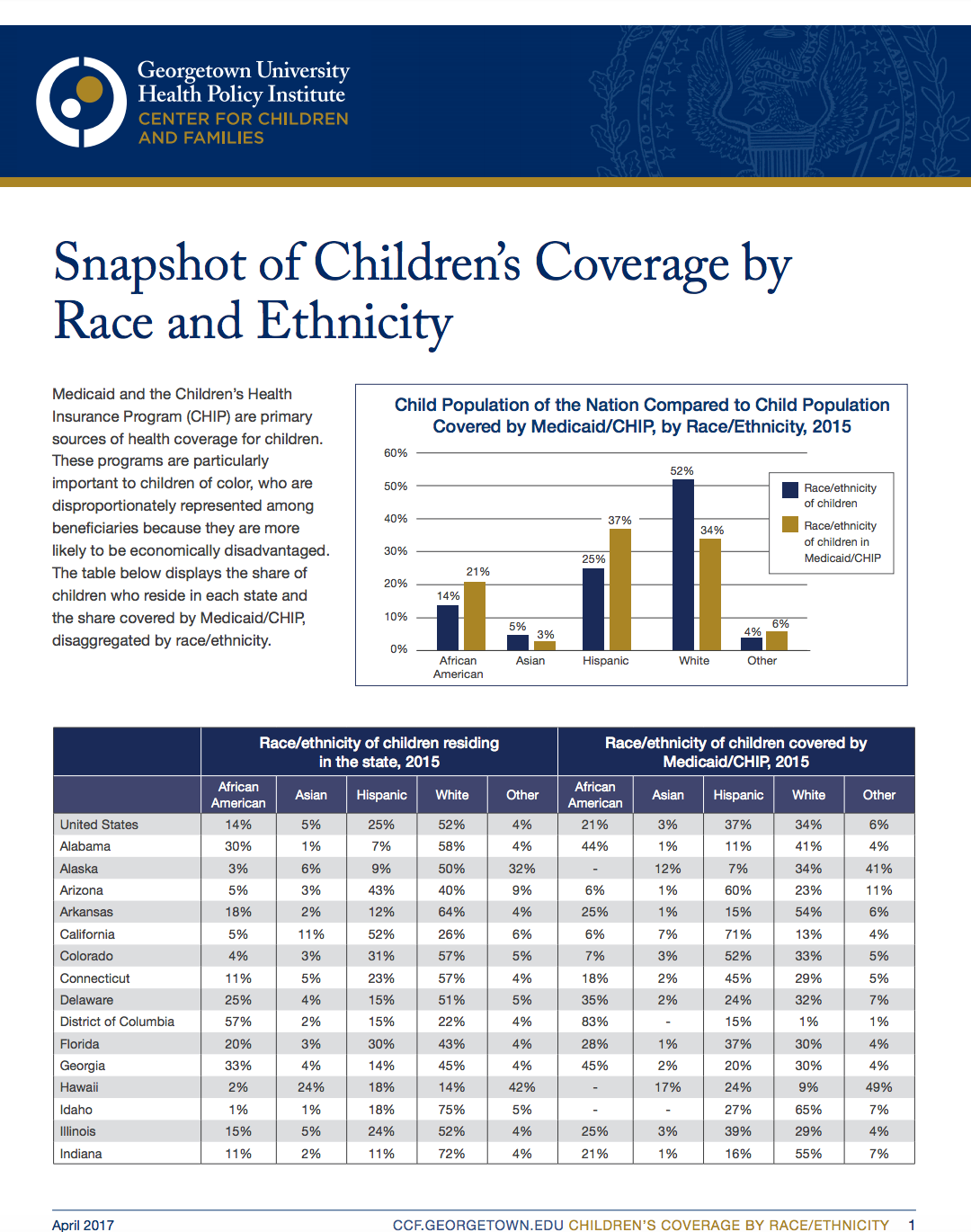
Medicaid And CHIP Help Address Racial/Ethnic Disparities In Children’s Health
Medicaid and CHIP are primary sources of health coverage for all children. These programs play a particularly important role for children of color, who are disproportionately represented among beneficiaries because they are more likely to be economically disadvantaged (see figure below). CCF’s new fact sheet unpacks child population and Medicaid/CHIP data by state. We know…
-
Snapshot of Children’s Coverage by Race and Ethnicity
Medicaid and the Children’s Health Insurance Program (CHIP) are primary sources of health coverage for children. These programs are particularly important to children of color, who are disproportionately represented among beneficiaries because they are more likely to be economically disadvantaged. (View our 2018 snapshot of children’s coverage by race and ethnicity.)
-
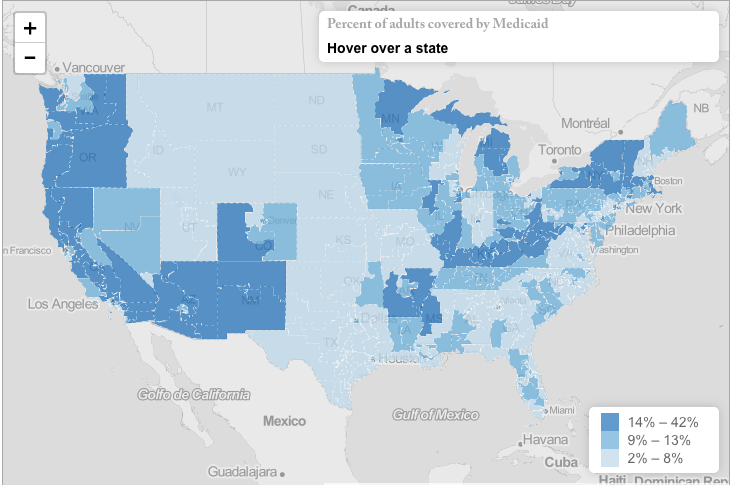
New Maps Display Medicaid/CHIP Enrollment by Congressional District
We have a new interactive map feature on our website and are excited to share with you the first maps we have created with our new tool. The maps visually display how Medicaid and the Children’s Health Insurance Program (CHIP) are helping to meet the needs of children and families across the country. You can…
-
New Efforts to Cut Medicaid and Repeal ACA Emerging in Congress
There are non-alternative reports that the White House and the Republican Congressional leadership are planning for a vote next week on legislation to “repeal and replace” the Affordable Care Act (ACA). Details as to what that legislation actually says are not yet available, but it’s likely that it will contain a cap on federal Medicaid…
-
Medicaid & CHIP are Long-Term Investments in Children’s Health and Future Success
As readers of Say Ahhh! know, Medicaid and the Children’s Health Insurance Program (CHIP) provide health coverage to more than one-third of the children in the United States and the vast majority of these children are covered through Medicaid. Our new report, Medicaid is a Smart Investment in Children, reviews the research on the long-term…
-
Survey Offers More Proof that Dental Coverage Counts
This was initially posted on the Children’s Dental Health Project blog by Matt Jacob A new national survey of U.S. parents shows that children without dental insurance were twice as likely as insured kids to have had a recent toothache or other dental problem that affected their ability to eat, sleep or concentrate in school. The…
-
AAP’s Bright Futures Takes Step Forward to Incorporate Social Determinants of Health
A child’s healthy development is influenced by access to health care but also by the social and physical environment in which the child lives. There is clear scientific evidence that children who live in safe, stable, and nurturing environments are more likely to thrive. And now pediatrician-developed preventive care guidelines for children have caught up…
-
Efforts to Repeal ACA and Cap Federal Medicaid Funding Fail
Today the mad dash efforts to repeal the Affordable Care Act and radically restructure Medicaid came to an abrupt halt when Speaker Paul Ryan and President Donald Trump were unable to garner enough votes to pass the American Health Care Act. This bill had taken a sharp detour from the normal path to the floor…
-
What’s at Stake if Essential Health Benefits are Scrapped? Pediatric Benefits, Protection from Lifetime Limits
As House leaders scramble to get enough votes to send the American Health Care Act to the Senate, there is a lot of horse-trading going on. None of it to the benefit of kids enrolled in Medicaid or private insurance. The most recent Affordable Care Act provision on the chopping block is the Essential Health…