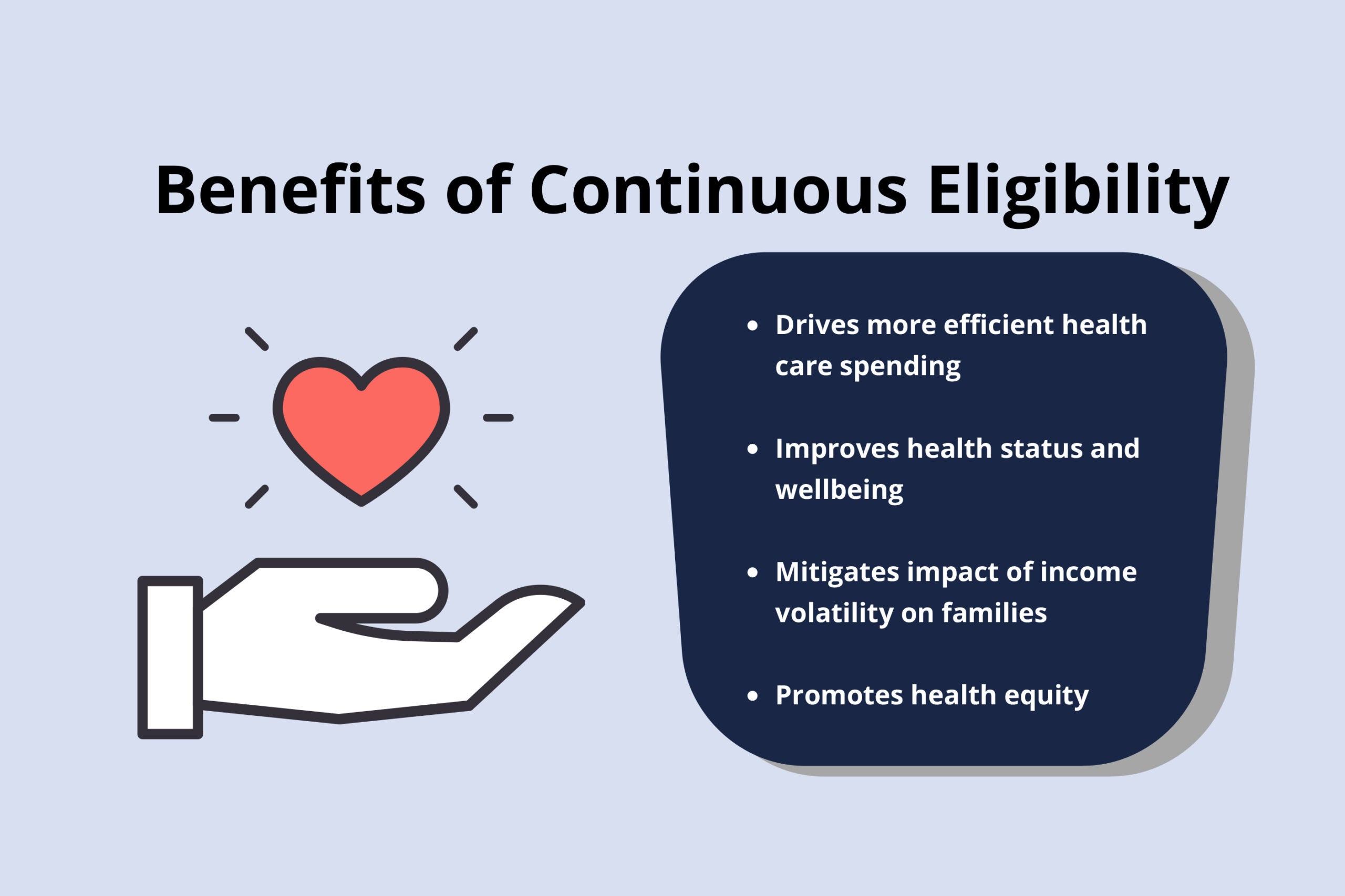
Continuous health insurance coverage produces a broad array of benefits across the health care sector for individuals, states, health plans, and providers. In particular, Medicaid continuous eligibility promotes health equity by limiting gaps in coverage for low-income children and adults who experience disproportionate rates of health disparities. Consistent access to health care, including management of chronic conditions and care coordination, improves health status and well-being and drives more efficient health care spending. Importantly, continuous eligibility better aligns with the realities faced by low-wage earners and essential workers. It mitigates the negative effects of income volatility and prevents disruptions in health care. By reducing the administrative costs associated with people cycling on and off of Medicaid due to temporary fluctuations in income, states can dedicate more of the Medicaid dollar to pay for health care. Moreover, continuous eligibility is necessary to fully measure the quality of health care in Medicaid and the Children’s Health Insurance Program (CHIP), which provides states with better tools to hold health plans and providers accountable for quality and improved health outcomes.
Currently, Medicaid is operating under the COVID public health emergency (PHE) provisions and all who are enrolled are protected by the continuous coverage provision. The PHE is widely expected to continue through the entirety of 2021, if not longer. But as states resume normal operations post-PHE, many individuals will lose the benefit of this continuous coverage. Under current law, states have limited continuous coverage requirements and state plan options in Medicaid and CHIP. Pregnant individuals in Medicaid must be continually covered through pregnancy until 60-days postpartum, and their infants must be continuously covered for one year. States may also opt to cover children for up to a full year, regardless of income fluctuations, through a straightforward state plan amendment (SPA). Starting in April 2022, states will also have a SPA option to extend coverage post pregnancy for one year. However, in order to extend continuous coverage to other eligibility groups, states must seek section 1115 demonstration authority from the federal government, an uncertain process that can be administratively complex, time-consuming, costly, and by no means assured.
CCF’s newest brief in its Future of Children’s Health Coverage series, “Continuous Eligibility in Medicaid and CHIP,” provides an update on the current policy landscape and benefits of continuous eligibility. It describes administrative actions that promote continuity of coverage at renewal, and during the year between renewals. It also recommends policy strategies to build on the success of continuous coverage in Medicaid such as:
- guaranteeing full year coverage for all children;
- allowing states to provide multi-year continuous eligibility for children without a section 1115 waiver;
- extending federal continuous eligibility requirements following pregnancy from 60 days to 12 months; and
- creating a new state option to extend 12-month continuous eligibility to adults.
There will likely be important lessons to be learned by examining enrollment patterns before, during, and after the PHE. As states develop their plans for resuming normal eligibility and enrollment operations post-pandemic, it is critically important to take appropriate steps to maintain ongoing coverage for all eligible individuals. Moreover, the end of the PHE is an ideal time to take stock of opportunities in Medicaid and CHIP to expand continuous eligibility policies and implement administrative processes that have proven to promote continuity of coverage.