Executive Summary
In the third year of the COVID-19 public health emergency (PHE), Medicaid enrollment continued to increase albeit at a slower pace than in the first two years of the coronavirus pandemic. Since March 2020, states have provided continuous enrollment in Medicaid in exchange for enhanced federal funding. This continuous enrollment provision and enhanced federal funding were originally in place until the end of the COVID-19 public health emergency (PHE). In December 2022, the Consolidated Appropriations Act, 2023 (CAA) delinked the provision from the PHE and ends continuous enrollment on March 31, 2023. Beginning April 1, 2023, states may restart disenrollments after conducting a full review of eligibility. States that follow all federal Medicaid renewal requirements, take steps to update enrollee contact information, and attempt to reach enrollees via non-mail modes before terminating coverage for returned mail will qualify for ongoing enhanced federal funding that phases down until the end of 2023. States must also report to the federal government specific data needed to monitor the impact of the unwinding or risk financial penalties for not doing so.
As states begin to “unwind” the continuous enrollment provision, many people will likely be found to be no longer eligible for Medicaid. Others could face administrative barriers and lose coverage despite remaining eligible. Existing state enrollment and renewal procedures, as well as state approaches to the unwinding of the continuous enrollment provision, will have major implications for Medicaid enrollment and broader coverage. Some states are prioritizing maintaining coverage by implementing the unwinding more slowly and taking steps to make it easier for people to renew coverage, while others are emphasizing a quicker end to continuous enrollment that reduces budgetary costs.
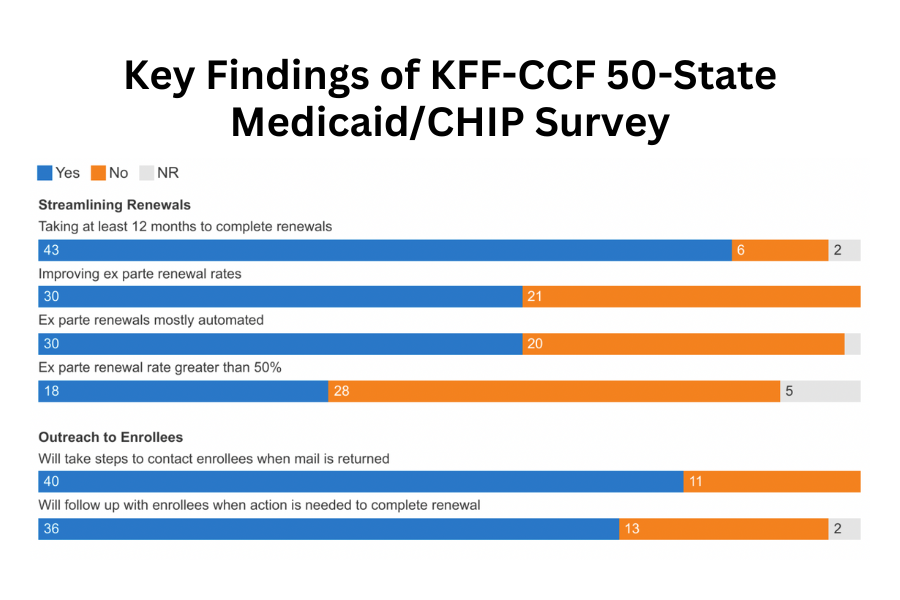
The 21st annual survey of state Medicaid and CHIP program officials conducted by KFF and the Georgetown University Center for Children and Families in January 2023 presents a snapshot of actions states are taking to prepare for the lifting of the continuous enrollment provision, as well as key state Medicaid eligibility, enrollment, and renewal policies and procedures in place as of January 2023. The report focuses on policies for children, pregnant individuals, parents, and other non-elderly adults whose eligibility is based on Modified Adjusted Gross Income (MAGI) financial eligibility rules. All states and the District of Columbia responded to the survey, although response rates for specific questions varied.
Introduction
Throughout 2022, the coronavirus public health emergency continued to have significant impacts on states. Since its emergence in early 2020, the coronavirus’ dual economic and public health crises continued to expose significant disparities in the public health infrastructure and further highlighted the importance of health coverage. Provisions in the Families First Coronavirus Response Act (FFCRA) and the Coronavirus Aid, Relief and Economic Security Act (CARES), required states to maintain eligibility and enrollment standards and provide continuous enrollment in Medicaid until the end of the public health emergency (PHE) to qualify for a 6.2 percentage point increase in Federal Medical Assistance Percentage (FMAP). During this time, states also adopted temporary changes in their state Medicaid plans through disaster-related authorities and temporary waivers to streamline processes and connect individuals to coverage more quickly, such as by expanding the use of presumptive eligibility, waiving premiums and cost-sharing, and allowing self-attestation of certain eligibility criteria. Largely due to the continuous enrollment provision, KFF estimates that Medicaid and CHIP enrollment will have grown by 23.3 million or over 30% by the time the continuous enrollment provision ends.
The Consolidated Appropriations Act (CAA), enacted in December 2022 delinked the continuous enrollment provision from the PHE, ending continuous enrollment on March 31, 2023. The CAA also phases down the enhanced FMAP through December 2023; states must meet certain maintenance of eligibility, data reporting, and other requirements to continue to qualify for the enhanced funding. CMS quickly released additional guidance on January 5, 2023 and January 31, 2023 on changes enacted by the CAA), in addition to providing technical assistance to states throughout 2022.
In this context and just after the CAA passed, KFF and the Georgetown University Center for Children and Families (CCF) fielded the 21st annual survey of Medicaid and CHIP program officials in the 50 states and the District of Columbia (DC) in January 2023. In anticipation of the end of the continuous enrollment provision, this year’s survey focuses on actions states are taking to prepare. It also provides data on state Medicaid and CHIP eligibility levels and presents a snapshot of key aspects of state enrollment and renewal procedures in place as of January 2023. The report focuses on policies for children, pregnant individuals, parents, and other non-elderly adults whose eligibility is based on Modified Adjusted Gross Income (MAGI) financial eligibility rules; it reports only limited policies for groups eligible through Medicaid pathways for adults over the age of 65 or on the basis of disability. All states responded to the survey although response rates for specific questions varied. The District of Columbia is counted as a state for purposes of this report.