All
-
Medicaid Managed Care Financial Transparency: Which States Are High Performers?
As Say Ahhh! readers know, CCF researchers have scanned state Medicaid agency websites for information about the performance of individual managed care organizations (MCOs) for children, for children and youth in foster care, and, most recently, for pregnant and post-partum women. In most of the states we looked, it wasn’t possible to identify which MCOs…
-
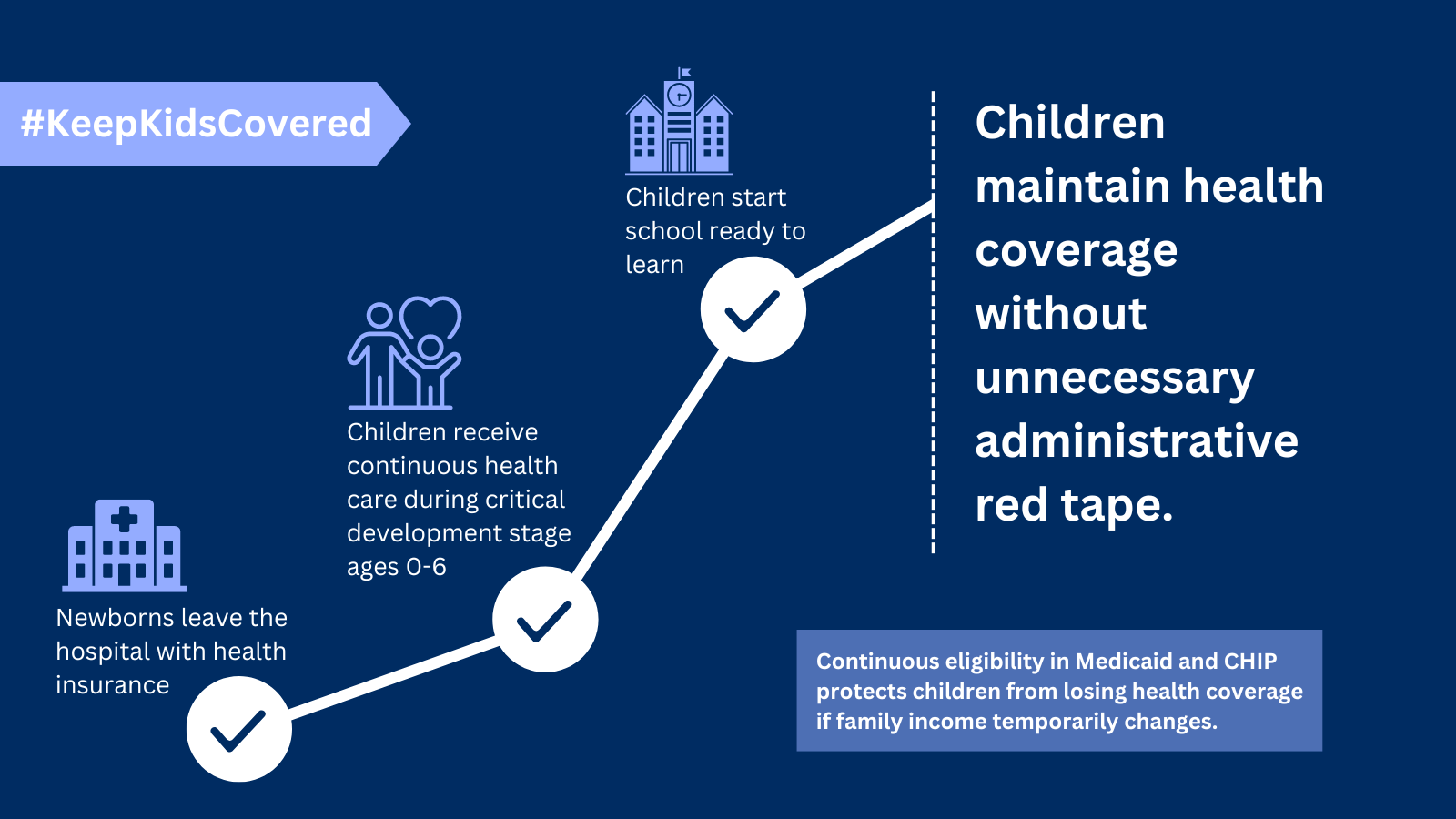
State of Florida Files Legal Challenge to Weaken Continuous Coverage Protection for Children in CHIP Nationwide
On February 1, the State of Florida filed a lawsuit in federal court in Tampa against the Centers for Medicare & Medicaid Services in an effort to prevent the agency from enforcing 12-month continuous eligibility in the state’s CHIP program. As loyal readers of Say Ahhh! know, the Consolidated Appropriations Act of 2023 required that…
-
Webinar: State Medicaid Opportunities to Support Mental Health of Mothers and Babies During the 12-Month Postpartum Period
Forty-six states and the District of Columbia have either implemented or plan to implement the state option to extend Medicaid coverage to all enrolled pregnant people from 60 days to 12 months following a pregnancy. In January, Georgetown CCF released State Opportunities to Support Mental Health of Mothers and Babies During the 12-Month Postpartum Period,…
-
CMS Releases Updated Medicaid & CHIP Telehealth Toolkit, Includes State Best Practices and Behavioral Health Strategies
This month, CMS released an updated State Medicaid and CHIP Telehealth Toolkit consolidating information from previous toolkits and providing additional guidance – as required by the Bipartisan Safer Communities Act – on issues from billing best practices to strategies for using telehealth in schools. In addition to FAQs on issues such as benefit flexibility, financing,…
-
If You Love Children, You Should Love these Medicaid/CHIP Policy Changes in 2024
Before the new year slips from memory, I wanted to take stock of a few good things happening for kids covered by Medicaid and CHIP this year. Amidst all the dismal news about how nearly 4 million children have lost their coverage during the unwinding – many remain eligible but lost coverage due to red…
-
Medicaid Managed Care: Results of the PHE Unwinding for the Big Five in Q4 2023
Q4 2023 was also the third quarter of the PHE “unwinding”—the redetermination of eligibility for all 86.7 million Medicaid enrollees following the expiration of the Public Health Emergency continuous coverage provision in March 2023. These redeterminations have resulted in the disenrollment of over 16 million Medicaid enrollees as of January 2024, which translates into a…
-
A Lifeline for Families of Children With Special Health Care Needs
By Gabby Benitez, Kristen Golden Testa and Nick Lutton Nine months after the start of a national effort to renew Americans’ Medicaid coverage, a tidal wave of people, including almost 200,000 children in California from June through October last year, lost their coverage – and an untold number may be joining them. Most disturbingly, this…
-
Marketplace Enrollment Surges Among Those Losing Medicaid Coverage During Unwinding
As readers of Say Ahhh! know, I have been tracking monthly data (here, here, here, here, here and here) from the Centers for Medicare and Medicaid Services (CMS) on the number of people who were either previously enrolled in Medicaid or had experienced a denial or termination during unwinding who then selected a marketplace plan. …
-
Medicaid Expansion in Georgia would Improve Maternal and Infant Health Outcomes
One in ten Georgians report knowing someone who has died through pregnancy-related causes. An estimated 57% of Georgians have experienced or know someone who has experienced maternal morbidity. Over 70% of Georgians believe that prioritizing improvements in access to health insurance coverage would help to reduce maternal mortality. These statistics were shared at the…
-
Where do Things Stand with Medicaid Unwinding at the Halfway Point?
KFF’s new research finds that states have reported outcomes for about half of Medicaid renewals nationwide, and so far 16.2 million people have been disenrolled. Meanwhile, our CCF tracker (which accounts for movement on and off the program as well as new enrollment by looking at net enrollment change in each state) shows a 9.37…
-
Minnesota Medicaid Revisits the Question: Managed Care or Fee-for-Service?
In the beginning, there was fee-for-service (FFS). In this case, the beginning was 1965, when Medicaid (and Medicare) were enacted. FFS was the way that these public programs, as well as almost all private insurers, purchased health care. Fast forward to today. Propelled by an interest in budget predictability and federal policy changes giving them…
-
Press Statement on Florida 12 Month Continuous Coverage for Children Lawsuit
Following is a statement by Joan Alker, executive director of the Georgetown University Center for Children and Families responding to a Florida lawsuit against a federal law requiring 12 months of continuous coverage for children enrolled in Medicaid or CHIP: “As a consequence of the Consolidated Appropriations Act of 2023, a new federal law went…
-
Multi-Year Continuous Eligibility for Children
As of January 1, 2024, all states are required to provide 12 months of continuous health coverage for children in Medicaid and the Children’s Health Insurance Program (CHIP). This reduces the risk of eligible children losing coverage due to administrative barriers or temporary fluctuations in family income. In 2022, Oregon became the first state approved…
-
Research Shows Medicaid Expansion Beneficial to Child Health and Family Financial Security
While the Affordable Care Act’s Medicaid expansion was designed to help the large number of uninsured adults who could not afford private insurance, the policy change has proven to be immensely helpful to children too. In February 2021, we released a report on the critical link between Medicaid expansion for adults and improvements to child…
-
It’s Unanimous: CMS Needs to Bring More Transparency to Medicaid Managed Care
Last week, MACPAC Commissioners voted to recommend that the Centers for Medicare & Medicaid Services post all state Managed Care Program Annual Reports (MCPARs) to the CMS website. The vote was unanimous: 17-0. The recommendation will be included in MACPAC’s March 2024 Report to Congress. At first glance, this may seem unremarkable, but on further…
-
CCF Comments on Questions from the Task Force on Maternal Mental Health
The Georgetown University Center for Children and Families submitted the following comments to the Office on Women’s Health at the U.S. Department of Health and Human Services regarding questions from the task force on maternal mental health. Read the Comments
-
CCF Comments on the Interim Final Rule on CMS Compliance with Reporting and Federal Medicaid Renewal Requirements
The Georgetown University Center for Children and Families submitted the following comments to the Centers for Medicare & Medicaid Services regarding the interim final rule on CMS enforcement of state compliance with reporting and federal Medicaid renewal requirements under Section 1902(tt) of the Social Security Act (CMS- 2447). Read the Comments
-
Momentum for Community Health Workers in Medicaid Continues in the New Year
For some good news to start 2024, the gains for community health workers (CHWs) in the Medicaid world continue to increase. We’ve written about the value of Medicaid as a sustainable funding source for CHW services and growing efforts in states previously here on Say Ahhh!…but wait, there’s more! Michigan has integrated CHWs in targeted…
-
Most States Show Improvement in Automated (Ex Parte) Medicaid Renewal Rates
Although ex parte was hardly a household term before the unwinding of the Medicaid continuous enrollment requirement, most stakeholders and observers are now aware of the critical role automating renewals using data available to the state can play in reducing churn and promoting continuity of coverage in Medicaid and CHIP. The policy not only removes…