CHIP
-
Mandatory Reporting on Medicaid Quality Measures: What Did Congress Intend?
In August, CMS posted its proposed rule to codify Congressional action taken in 2018 to mandate state reporting of the Child Core Set and the Adult Behavioral Health Core Set of quality measures in Medicaid and CHIP, starting in 2024. Until 2024, state reporting on the core sets is voluntary. I did a quick scan…
-
Webinar: Medicaid Continuous Eligibility for Children up to age 6 in Oregon
On September 28, CMS approved Oregon’s groundbreaking proposal to provide continuous eligibility (CE) in Medicaid and CHIP for children from birth to age 6 as a component of the state’s school readiness and health care transformation strategies. The approval also creates a two-year CE for all beneficiaries ages 6 and older, along with a number…
-
Proposed Rule Offers Opportunity to Help Advance Maternal Health Equity
We can’t improve what we don’t measure. That’s why it is important for all who want to improve maternal and child health to take a look at a proposed rule now up for comment that provides an important opportunity to increase transparency and accountability for the quality of care delivered through Medicaid and CHIP. The…
-
Oregon Leads the Nation By Covering Children in Medicaid from Birth to Kindergarten – Which State Will Be Next??
The Biden Administration announced today that it will approve Oregon’s request to provide continuous Medicaid coverage to children from birth through age five and for two years for all Oregonians enrolled in Medicaid age six and up. This use of Section 1115 authority is precisely what Medicaid demonstrations are for — as we and colleagues…
-
Biden Administration Releases Final Rule on Public Charge
After years of seemingly ever-changing rules around public charge, it comes as a relief to see a final rule that is faithful to the statute and supported by extensive policy evidence. The definition of public charge in the final rule is consistent with long established public charge policy and law, unlike the rules under the…
-
Research Shows More Can Be Done to Ensure Eligible Immigrant Children and Families Get Access to Health Coverage
Since 2009, states have had the option to extend Medicaid and CHIP eligibility to lawfully residing immigrant children and pregnant people without a five-year waiting period through what is known as ICHIA (a reference to a 2007 bill called the Immigrant Children’s Health Improvement Act) or CHIPRA §214 (a reference to the section of the…
-
Proposed Eligibility Rule Simplifies Medicaid and CHIP Enrollment Process for Children
In a continuing effort to strengthen Medicaid and access to affordable, quality health coverage, the Biden Administration has proposed a series of eligibility rule changes. The Notice of Proposed Rulemaking (NPRM) seeks to streamline application and enrollment, improve retention rates, remove barriers specific to CHIP, and enhance program integrity. Eliminates enrollment barriers and benefit caps…
-
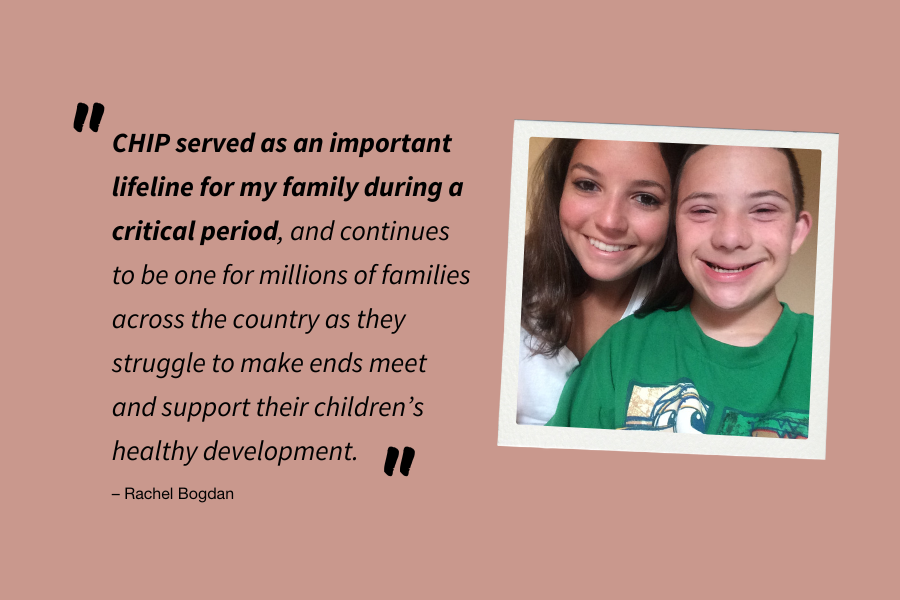
CHIP Helped My Family Through a Tough Time
We often hear “it takes a village to raise a child” and that adage certainly holds true for my childhood. I am the third oldest in a large family. My parents worked different shifts so one of them could usually be home with us while my grandparents filled in the gaps. Additionally, my two older…
-
Long-Awaited Rule on Mandatory Reporting of Child Core Set Quality Measures Proposed
Yesterday, CMS released its Notice of Proposed Rulemaking (NPRM) on the Child Core Set of Health Care Quality Measures in Medicaid and CHIP (known as the child core set). The proposed rule will implement the mandatory reporting of the child core set in 2024 as required by the Bipartisan Budget Act of 2018. The NPRM,…
-
CMS Reminds States EPSDT Requirement Includes Behavioral Health, Offers Specific Strategies
Medicaid’s pediatric benefit, Early and Periodic Screening Diagnostic and Treatment (EPSDT), is getting more attention from federal officials. As part of its child health-focused release yesterday, CMS released a new Informational Bulletin reiterating EPSDT’s requirement to cover screenings and medically necessary treatment for children’s behavioral health, mental health and substance use disorders. The timing is…
-
Children’s Health and Well-Being Get Much Needed Attention from CMS this Week
CMS made three big announcements yesterday, drawing attention to ways Medicaid and CHIP can support children’s health and well-being. The first two announcements are sub-regulatory guidance documents, essentially bringing together all of the existing state options and best practices on behavioral health and school-based health. Sub-regulatory guidance doesn’t include new policy, but rather aims to…
-
Bipartisan Safer Communities Act Greenlights Updated School-Based Medicaid Guidance, TA Center and Grant Funding
On June 25, President Biden signed the Bipartisan Safer Communities Act into law. While a high-level overview of the legislation has previously been detailed on SayAhhh!, with the language now enacted into law, we thought it would be helpful to drill down into more detail on the provisions relating to Medicaid and CHIP and school-based…
-
Opportunities to Support Maternal and Child Health Through Medicaid’s New Postpartum Coverage Extension
Introduction The new state option to extend Medicaid and CHIP coverage for one year after the end of pregnancy is a transformational opportunity for states to support improved maternal and infant health in the year following birth. It also offers state Medicaid leaders a focused moment to use the successful implementation of the new policy…
-
CHIP: Serving America’s Children for 25 Years
In its 25-year history, the Children’s Health Insurance Program (CHIP) has established itself as a critical piece of the federal-state response to children’s health care needs. CHIP, signed into law on August 5, 1997, was created to build on the success of Medicaid by giving states the opportunity to receive enhanced federal matching funds to…
-
Infants Covered by Medicaid and CHIP Likely Hardest Hit by Formula Shortage, WIC a Key Resource
Before newborns can try solid foods, breastmilk or infant formula are the sole sources of nutrition to keep them fed. This is why the infant formula shortage has added yet another layer of stress on families with infants. As many families continue to struggle to access formula, a new brief from the Kaiser Family Foundation…
-
New Urban Institute Analysis Underscores Importance of Continuous Medicaid Coverage Protection for Kids
A new brief out this week from The Urban Institute confirms what we have suspected — the Medicaid continuous coverage provision has halted the increase in uninsured children that we saw during the Trump years. (As SayAhhh! readers know, no one can be involuntarily disenrolled during the federally declared public health emergency as a consequence…
-
New Data from CMS Shows Mental Health Services for Children Continue to Lag Behind Pre-Pandemic Levels
This week, the Centers for Medicare & Medicaid Services (CMS) released an update to its Medicaid and CHIP COVID-19 data snapshot with new data through January 2022. Unfortunately, as highlighted in the snapshot, while the number of mental health services provided to adults during the public health emergency nearly returned to pre-pandemic levels, the rate…
-
CMS Affirms States Must Cover Stand-Alone Vaccine Counseling under EPSDT, More Work to Be Done
As families and parents across the country eagerly await approval of the COVID-19 vaccine for children under 5, new guidance from CMS reaffirms that states must cover stand-alone vaccine counseling for children covered by Medicaid under EPSDT. According to guidance released last week, CMS reiterates that under Medicaid’s Early and Periodic Screening, Diagnostic, and Treatment…
-
How Medicaid Can Help Schools Sustain Support for Students’ Mental Health
Among the Covid-19 pandemic’s most pernicious aftershocks is its impact on student mental health. Isolated at home, disconnected from friends, and suffering trauma from family members’ job losses or Covid-related deaths, students are experiencing high levels of anxiety and depression. About 44 percent of adolescents experienced persistent feelings of sadness or hopelessness during the pandemic compared to…
-
More Children Enrolled in ACA Marketplace Coverage in 2022, But Marketplaces Still Remain Modest Source of Health Coverage for Children
Medicaid and the Children’s Health Insurance Program (CHIP) currently cover more than 40 million children. In comparison, relatively few children rely on the marketplaces for their health coverage. But new data released by the Centers for Medicare & Medicaid Services (CMS) show 1.3 million children were enrolled in marketplace plans during the 2022 Marketplace Open…