Medicaid
-
Missing Out On New Health Coverage: Four States Where The Debate Around The GOP’s Health Care Bill Is Hurting Efforts To Close The Medicaid Coverage Gap
While the ultimate outcome for the GOP health care bill is unclear here in Washington, the uncertainty created by the legislation is already having an adverse effect on attempts to expand coverage in four states. Idaho, Georgia, Tennessee, and Kansas all have had robust discussions over the past year about joining the other 32 states…
-
Health Proposal Breaks Long-standing Bipartisan Commitment to Children’s Health
With virtually no time to unpack the provisions in the Manager’s Amendment that was released late Monday night and no CBO score expected until just before the vote, it appears that the House is on the verge of voting to repeal not just the Affordable Care Act, but also break the long-standing bipartisan promise of…
-
Covering Parents Helps Kids
While historic progress has been made in lowering the number of uninsured children in the United States, the number of uninsured parents – almost 12 million in 2010—has soared as fewer employers offered their workers health insurance and strict eligibility limits were in place for adults in need of Medicaid coverage. The Affordable Care Act…
-
Health Coverage for Parents and Caregivers Helps Children
Children’s healthy development depends to a large extent on the health and well-being of their parents and caregivers. Covering parents and caregivers helps children get the care and family financial stability they need to thrive.
-
Proposed Medicaid Spending Caps Rely on Data Points That Don’t Exist Yet
There were few details in the recent CBO score on the American Health Care Act (AHCA) as to how the $880 billion in cuts to Medicaid were calculated and where the pain will be felt. That’s because the folks at CBO, like the rest of us, are scratching their heads over where to access the…
-
New CMS Administrator Verma Takes The Helm And Reaches Out To Governors On Medicaid
On Monday night, the Senate confirmed the nomination of Seema Verma to head the Centers for Medicare and Medicaid Services (CMS) by a 55-43 vote. Verma, as Say Ahhh! readers know, comes to CMS from Indiana where she worked for then-Gov. Mike Pence as a consultant on the state’s Healthy Indiana program. As I expected,…
-
Follow the Money: CBO Shows House “Repeal and Replace” Bill is Really “Cap and Cut” Medicaid
On March 13 the Congressional Budget Office (CBO) issued its estimate of the House bill to “repeal and replace” the Affordable Care Act. The House bill does far more than simply “repeal and replace” the ACA Medicaid expansion for adults. It would end the federal government’s 50-year, open-ended commitment to all Medicaid populations — the elderly,…
-
How the AHCA Yanks Welcome Mat Out From Under Children Eligible for Medicaid and CHIP
The Affordable Care Act’s (ACA) coverage provisions did not target children’s eligibility for Medicaid or CHIP. It was aimed at closing the coverage gap for adults – both adults without dependent children, who were generally ineligible for Medicaid, and parents, whose pre-ACA Medicaid eligibility was well below the poverty level in many states. Yet, we…
-
How the Wrong Medicaid Reforms Could Devastate Young People with Complex Medical Needs
By Sophia Jan, Ahaviah Glaser, Rebecca Kim of Children’s Hospital of Philadelphia (CHOP) Policy Lab Current proposals to simultaneously repeal the Affordable Care Act (ACA) and reform the federal Medicaid program would be devastating to children and young adults with disabilities and complex medical needs. Even if the final ACA replacement plan continues to allow…
-
ARKids First turns 20!
Originally posted by Arkansas Advocates for Children and Families. Twenty years ago today, on March 10, 1997, then-Arkansas Governor Mike Huckabee signed ARKids First into law. ARKids was Arkansas’s state-funded health insurance program, and bringing it to life was a monumental moment for kids and families in our state. ARKids filled in the gap for…
-
Impact of Medicaid on Children: Latest Research Findings
Medicaid and the Children’s Health Insurance Program (CHIP) provide health coverage to more than one-third of the children in the United States. The vast majority of these children, more than 90 percent, are covered through Medicaid. A large body of research shows that access to Medicaid in childhood leads to longer, healthier lives, a better chance to…
-
Medicaid Provides Economic Security For Families
Our new fact sheet summarizes research on how Medicaid provides economic security for families. By making health insurance accessible to children and parents, Medicaid keeps families healthy and also protects them from financial hardship. That economic security has the added benefit of insulating children from some of the adverse experiences of growing-up in poverty that…
-
Up All Night
By Rylin Rodgers, Riley Child Development Center When was the last time you were up all night worrying about something? I hope you had to think hard in order to answer that one because it’s been a while. For most of us, though, it probably wasn’t that long ago. Most of us have the experience of…
-
Medicaid: How Does It Provide Economic Security for Families?
Research shows that Medicaid coverage improves numerous indicators of economic security for beneficiaries. By making health insurance accessible to children and parents, Medicaid keeps families healthy and also protects them from financial hardship. For millions of families, Medicaid is a lifeline that keeps them living above the poverty threshold.
-
Why “State Flexibility” Won’t Do the Trick to Implement Medicaid Cuts
There has always been a lot of overheated rhetoric about state flexibility in the Medicaid program, but at no point has it been more important to unpack that concept than now. With the House and Senate poised to act on a bill which caps the Medicaid program for the first time in its history, proponents…
-
What Does House ACA Repeal Proposal Mean for Children and Families?
As the House of Representatives moves with rapid speed to pass legislation to repeal the Affordable Care Act, the public can finally get a glimpse of their plan – though the public still needs a lot more information about the proposal and the “intended” and “unintended” consequences it would have for children and families. The…
-
ACA Repeal Would Also Impact Kids Who Get Health Coverage Through Parent’s Employer
We often talk about how Medicaid is the MVP for children’s coverage – and it is – covering 37 million children today in Medicaid directly plus over half of children whose coverage is paid for by CHIP, for a total of 42 million kids. But if you look at public and private sources of coverage,…
-
House GOP Medicaid Provisions Would Cut Federal Medicaid Spending by $560 Billion Over Next Decade
By Edwin Park, CBPP The House Republican health plan would shift an estimated $560 billion in Medicaid costs to states over the next ten years, effectively ending the Affordable Care Act’s (ACA) Medicaid expansion for 11 million people while also harming tens of millions of additional seniors, people with disabilities, and children and parents who rely on…
-
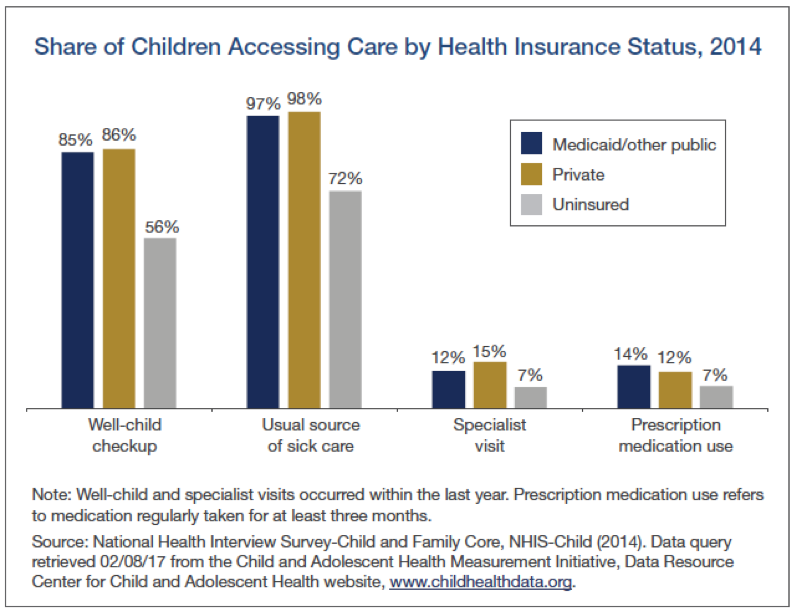
New CCF Fact Sheet Shows Medicaid Provides Needed Access to Health Care for Families
Our new fact sheet summarizes research on access to care in Medicaid. We find that children and parents who rely on Medicaid for health care receive coverage that is comparable to private insurance and far better than the access accorded uninsured families. Children covered by Medicaid and those with private insurance access health care services…