2023
-
Child Medicaid Enrollment Decline Reaches 3 Million: How Many Kids are Moving to CHIP?
Our tracker of net child Medicaid enrollment declines during the unwinding period just reached, and then quickly exceeded, 3 million with the release of October data by Texas – the undisputed national leader in dumping kids off Medicaid. In February 2022, Georgetown CCF researchers projected that as many as 6.7 million children could experience a…
-
Program Assistant
The program assistant will provide research and administrative support to CCF, primarily but not exclusively to the Center’s maternal and early childhood team. This position requires a high level of competence and commitment, interest in health policy that addresses health equity, as well as a wide range of administrative, communications, and administrative management skills. The…
-
Zero to Six Continuous Coverage Proposed in Pennsylvania, Approved in New Mexico
As we hit the milestone of 3 million children losing Medicaid coverage in less than a year, movement toward multi-year eligibility in Medicaid continues to be a bright spot in the unwinding storm. Last week CMS approved New Mexico’s request to implement continuous coverage for children up to age 6, joining Oregon and Washington in…
-
As Extra Medicaid Funding Phases Out at Year’s End, States Must Still Report Data and Comply with Federal Renewal Requirements
Starting in 2024, states will no longer receive extra federal funding associated with the Medicaid continuous enrollment requirement that was in place from March 2020 through March 2023. But the recent Interim Final Rule with Comment (IFC) released by CMS reminds states that they must continue to meet data reporting requirements specified by Congress and…
-
A 1-2 Policy Punch Would Earn States a Gold Star in Covering Kids
As CCF’s Medicaid child enrollment tracker hit a sobering milestone this week – a net decline of 3 million children since March 2023 – CMS released a package of documents advising and encouraging states to do more to make sure children don’t slip through the cracks during the unwinding of the pandemic-related continuous enrollment requirement.…
-
New Report Finds Alarming Trends in Maternal and Infant Health in Idaho and Calls for Improvements to Health Care Access
By Ivy Smith, Health Policy Specialist at Idaho Voices for Children Infant mortality in Idaho rose 18% and maternal mortality rose a staggering 121.5% from 2019 to 2021, according the Idaho Maternal and Infant Health Report 2023 published by Idaho Kids Covered, a statewide coalition of health care advocates and stakeholders supported by Idaho Voices…
-
Transitional Medical Assistance (TMA) and the Unwinding
Late last month, CMS released long-awaited guidance on Medicaid coverage for low-income working parents in the context of the unwinding of continuous coverage. Technically, this coverage is a mandatory eligibility category known as transitional medical assistance, or TMA, because it was originally designed to help parents transition from Medicaid to private insurance coverage through the…
-
House Passes Bipartisan Medicaid and CHIP Behavioral Health Provisions, Senate Committees Act: Here’s a Breakdown
Last week, the House of Representatives passed its Support for Patients and Communities Reauthorization Act. Passing on a broad bipartisan basis, the bill would reauthorize certain provisions of the 2018 SUPPORT Act such as those supporting individuals with substance use disorders (SUDs) like requiring state Medicaid programs to provide coverage for medication-assisted treatment in addition…
-
Three Million Fewer Children in the U.S. are Covered by Medicaid: CHIP Enrollment Isn’t Growing Much
As readers of Say Ahh! know, we’ve been closely tracking data from around the country related to the lifting of the COVID-19 pandemic related continuous coverage protections in Medicaid. The tracker is going up very quickly now– we hit one million on Halloween, two million on Thanksgiving and today three million fewer children are enrolled…
-
A Tipping Point for School Medicaid Expansion
By Jessie Mandle, National Program Director of the Healthy Schools Campaign Since 2014, school districts have been allowed to bill Medicaid for all health services provided to all Medicaid-enrolled students, instead of being limited to reimbursement for services included in a student’s Individualized Education Plan (IEP). However, states have been slow to leverage this opportunity…
-
Transparency in Medicaid Managed Care: The Wait Goes On
Last month, the Centers for Medicaid & CHIP Services (CMCS) issued a Center Informational Bulletin, “Medicaid and CHIP Managed Care Monitoring and Oversight Tools.” Among other items, this CIB discusses the Managed Care Program Annual Reports that state Medicaid agencies are required to submit to CMS. MCPARs are each state’s accounting of how each of…
-
Medicaid Managed Care in 2023: The Year that Was
2023 marked an inflection point in the growth of Medicaid managed care. Enrollment in MCOs, which had climbed continuously in both 2021 and 2022 due largely to the continuous coverage policy in place during the Public Health Emergency, plateaued and then headed downward, due largely to the PHE unwinding. Much uncertainty remains as to how…
-
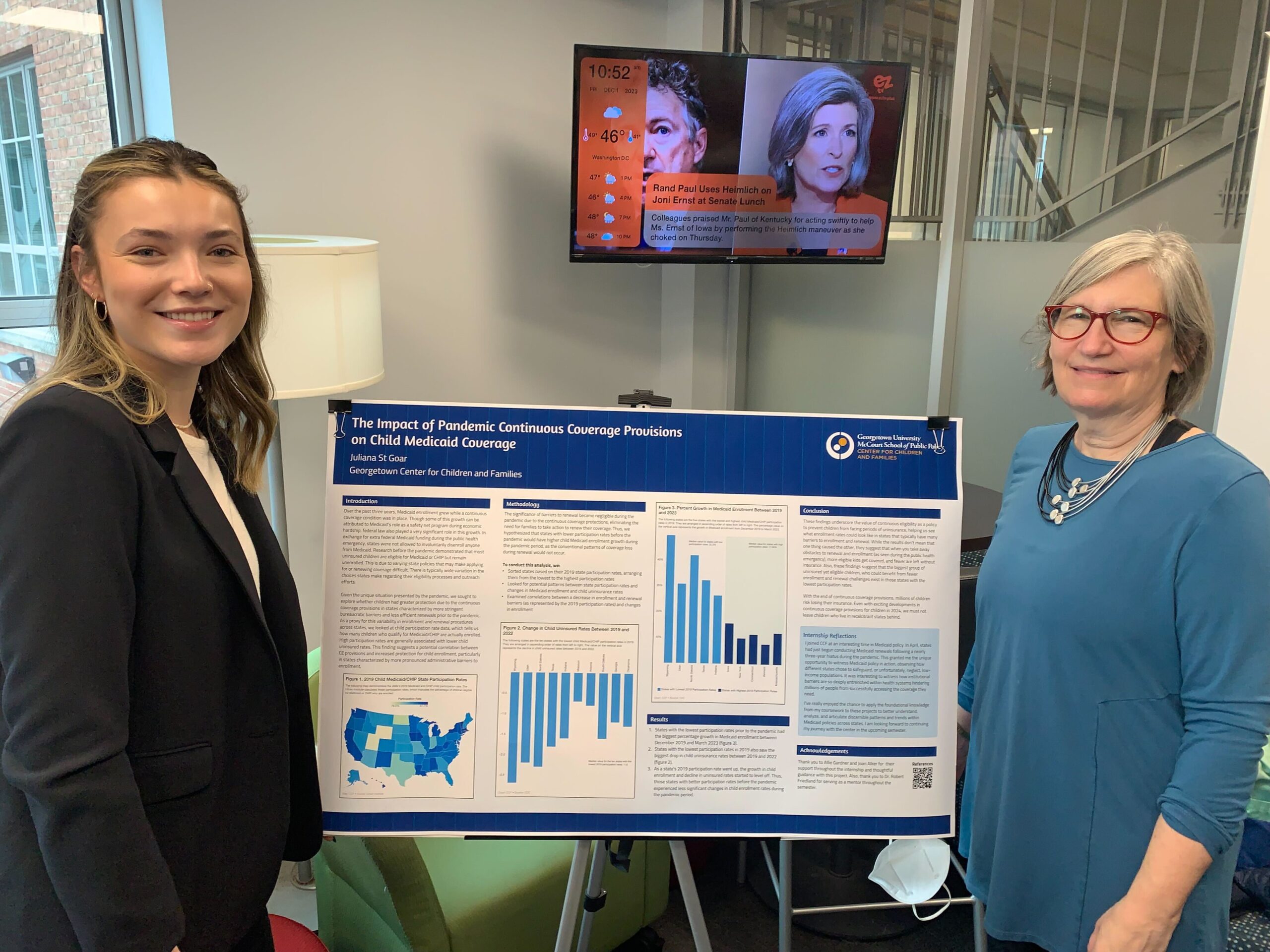
States with Low Medicaid Participation Rates Saw the Greatest Child Coverage Gains During the Period of Pandemic Continuous Coverage Protections
By: Juliana St Goar & Joan Alker It is well documented that over the past three years, Medicaid enrollment grew while a continuous coverage requirement was in place. Though some of this growth can be attributed to Medicaid’s crucial role as a safety net program during times of economic hardship, federal law also played a…
-
CCF Comments on Processes for Assessing Compliance with Mental Health Parity and Addiction Equity in Medicaid and CHIP
The Georgetown University Center for Children and Families submitted the following comments to CMS regarding the proposed processes for assessing compliance with mental health parity and addiction equity in Medicaid and CHIP. Read the Comments
-
Medicaid Expansion Enrollment Opens in North Carolina
On December 1, North Carolina became the latest state to expand Medicaid under the Affordable Care Act, meaning approximately 600,000 residents now have access to comprehensive health coverage. The North Carolina Department of Health and Human Services is now providing links and information on how to quickly apply for coverage either online, over the phone,…
-
In August, Marketplace Enrollment Slowed Among Those Losing Medicaid Coverage During Unwinding
As readers of Say Ahhh! know, I have been tracking monthly data (here, here, here, and here) from the Centers for Medicare and Medicaid Services (CMS) on the number of people who were either previously enrolled in Medicaid or had experienced a denial or termination who then selected a marketplace plan. CMS has just issued…
-
CMS Releases New Unwinding-Related Renewal Resources for Health Care Settings
CMS recently released a toolkit for clinical offices and health care settings with patient-centered messaging regarding the unwinding of the Medicaid continuous enrollment requirement. The toolkit includes helpful information on how health care providers can share information on Medicaid and CHIP renewals with patients. The toolkit starts with suggestions on what various staff members within…
-
Florida’s Rolling Out a New Medicaid/SNAP Portal Next Week – Throwing Gas on the Unwinding Fire
With little advance notice to the community, the state of Florida announced in mid-November that it was moving next week (December 5th) to a new portal for eligibility for Medicaid, SNAP, child care and TANF; and that every person/household in the state accessing those benefits will need to create a new account. Every person create…
-
Georgia Pathways Implementation: The Glass is 99.6% Empty
On October 5, 2023, CMS certified as complete Georgia’s implementation plan (the implementation plan itself starts on page 50) for phase one of its “Pathways to Coverage” section 1115 demonstration that the state had already started implementing more than 3 months earlier, on July 1, 2023. Yes, you read that right. And no, it doesn’t…
-
Biden Administration Says No to Premiums in Medicaid Again – This Time in Wisconsin
We’re getting to the end of the year and a seasonal tradition for Medicaid Section 1115 waiver watchers is observing an uptick in waiver activity by the federal Centers for Medicare and Medicaid Services (CMS). Last Friday, CMS issued a temporary one-year extension (in place until December 31, 2024) for Wisconsin’s BadgerCare Section 1115 demonstration…