All
-
Methodology for Report “Number of Uninsured Children Stabilized and Improved Slightly During the Pandemic”
Data Sources and Changes to Race/Ethnicity Questions and Age Categories for Children This report from the Georgetown University Center for Children and Families (CCF) uses data from the U.S. Census Bureau American Community Survey (ACS). The ACS randomly selects about 3.5 million households each year to be surveyed and conducts the survey year-round, publishing results…
-
Children’s Health Coverage Report Press Call
Listen to Press Call Read Press Release Speaker Bios for December 7, 2022 Press Call Joan Alker is the co-founder and executive director of the Georgetown University Center for Children and Families and a Research Professor at the Georgetown University McCourt School of Public Policy. She is a nationally recognized expert on Medicaid and…
-
Mapping the Barriers to Renewing Medicaid Coverage for Rural Arizonans When Continuous Coverage Ends
By Zaida Dedolph Piecoro and Bryna Koch Currently, half of those at risk of coverage loss at the end of the public health emergency (PHE) in Arizona are children under 19. Like many others, we at Children’s Action Alliance and our partners at the University of Arizona, Arizona Center for Rural Health are strategizing to…
-
Unwinding Wednesday #12: More States Are Taking Advantage of Flexibilities Aimed at Mitigating Gaps in Coverage during Unwinding
A few months ago, we wrote about new data from CMS on approvals of time-limited waivers, or (e)(14) waivers, that states may adopt to smooth the unwinding process and mitigate unnecessary gaps in coverage. Only 20 states had been approved for these temporary waivers at the time the data was initially released. Since then, the…
-
Number of Uninsured Children Stabilized and Improved Slightly During the Pandemic
Data released by the U.S. Census Bureau’s American Community Survey (ACS) for 2021 finds that nationally the estimated number and rate of uninsured children went down slightly from 2019 to 2021. This data provides the first comprehensive look at what happened to children with respect to this metric during the first part of the COVID-19…
-
States Can Help Address the Child Care Crisis by Prioritizing Health Coverage
Federal and state lawmakers are seeking policy solutions to address the child care crisis that was exacerbated by the pandemic. Workforce challenges loom large, with necessary attention to boost wages for the child care professionals who play a role in not only helping parents work, but also promoting early childhood development. But states can also…
-
State Opportunities to Improve Health Care Coverage for Child Care Professionals
States are grappling with how to more effectively support their child care workforce, including ensuring providers have access to affordable health care. Just like parents, frontline early education professionals are better able to support children in their care when they are healthy. A healthy caregiver is especially important for young children because brain development in…
-
New Report Highlights Role Medicaid Can Play in Advancing Comprehensive School Mental Health Services
Last month, the Healthy Schools Campaign and Mental Health America released a new report titled, “State Policy Opportunities: Advancing Comprehensive School Mental Health Systems to Support Students”, which provides a new perspective on the key actors that can play a role in advancing comprehensive school mental health systems for students. But what counts as a…
-
Federal Focus on Behavioral Health Crisis Care
You may be thinking that we’ve been writing a lot about behavioral health on Say Ahhh! lately. Well, you’re right – and there’s more! For starters, last week, the Substance Abuse and Mental Health Services Administration (SAMHSA) released new National Guidelines for Child and Youth Behavioral Health Crisis Care, complementing other recent resources such as…
-
Are Medicaid Enrollees Aware that Medicaid Renewals Will Restart Soon?
A new brief by the Urban Institute indicates that nearly two-thirds of adults (62 percent) who are covered by or have a Medicaid-enrolled family member are unaware that Medicaid renewals will be restarting in the future. Of those who had heard at least a little about the resumption of renewals, the largest source of information…
-
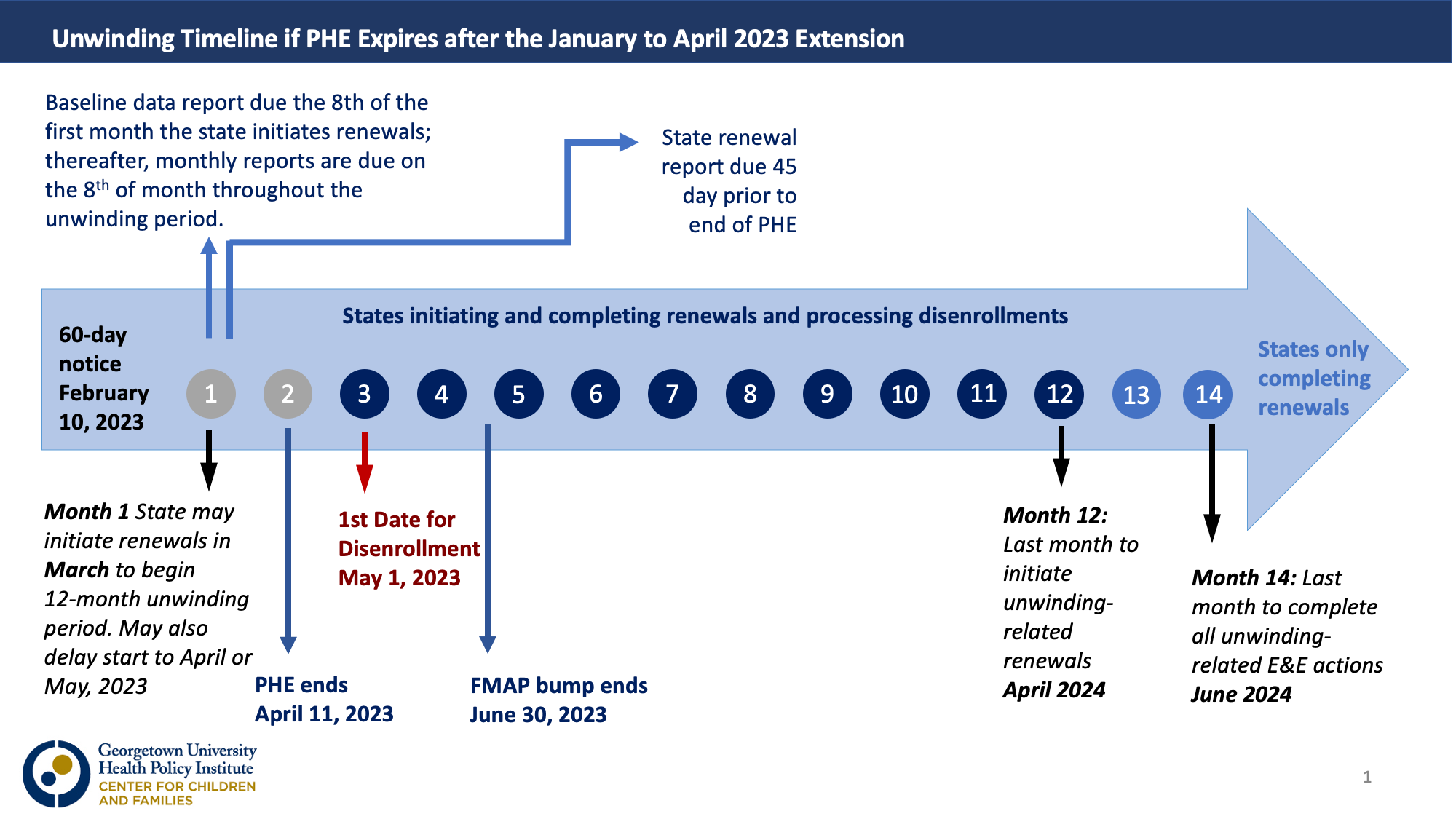
Unwinding Wednesday #11: No 60-day Notice on the Unwinding; PHE Expected to Be Extended Until April 2023
[Editor’s Note: The end-of-year bipartisan funding agreement released on December 20 would delink the continuous coverage requirement from the HHS Secretary’s declaration of a public health emergency and start the Medicaid “unwinding” process on April 1. The agreement includes 12 months of continuous coverage for children and other provisions designed to protect individuals eligible for…
-
States Leading the Way on Connecting All Children with Health Coverage – Will Congress Follow?
According to the Urban Institute, over half of the remaining uninsured children are eligible for Medicaid or the Children’s Health Insurance Program (CHIP) but unenrolled. About a third of uninsured children are ineligible for Medicaid or CHIP because their family income exceeds the eligibility thresholds. Another 10% are ineligible for Medicaid/CHIP because of their immigration…
-
Transparency in Medicaid Managed Care: The Power of the California Procurement Database
The Illinois Answers Project has just published a must-read piece of investigative reporting: “Insurance Giant Failed Foster Kids with Inadequate Care.” It raises a number of disturbing questions about the way children in foster care are being treated in the state’s Medicaid managed care program. About the performance of a Centene subsidiary that has contracted…
-
South Dakota Voters Pass Medicaid Expansion. What Happens Next?
South Dakota voters followed the pattern of six other states and voted this week to expand Medicaid, extending affordable health care to more than 40,000 adults largely working in jobs without health coverage like hospitality, food service, and construction. In taking this action, South Dakota now joins 39 other states and the District of Columbia.…
-
Unwinding Wednesday #10: FAQs Provide Additional Clarity on State Options Before and During the Unwinding
Over the past two years, CMS has published a wealth of resources designed to aid states in the unwinding process. These documents, which provide guidance and lay out flexibilities available to states, are available on a single landing page on Medicaid.gov. In our tenth installment of Unwinding Wednesday, we are highlighting a recent addition to…
-
Medicaid Managed Care: The Big Five in PHE Q11 (Q3 2022)
September 30 marked the end of the 3rd quarter of this calendar year. It also marked the end of the 11th quarter of the Public Health Emergency (PHE). The two are not unrelated. During the PHE, states receive an additional 6.2 percentage points on their regular federal matching rate if they agree not to terminate…
-
Comments on Streamlining Medicaid/CHIP Eligibility Determination, Enrollment and Renewal Processes
Georgetown University Center for Children and Families submitted these comments to CMS on the “Streamlining the Medicaid, Children’s Health Insurance Program, and Basic Health Program Application, Eligibility Determination, Enrollment, and Renewal Processes Proposed Rule.” EE NPRM CCF Comments
-
Comments on Amendments to “KanCare” Medicaid Demonstration
The Georgetown University Center for Children and Families and the Center on Budget and Policy Priorities submitted the following comments to CMS regarding Kansas’ application to amend the “KanCare” Medicaid demonstration that would authorize continuous eligibility for parents and caretaker relatives. KanCare Amendment Comments
-
Letter Regarding Healthy Michigan Plan Section 1115 Demonstration Extension Application
The Georgetown University Center for Children and Families and the Center on Budget and Policy Priorities sent this letter to CMS regarding Michigan’s application to extend its “Health Michigan” 1115 waiver. CCF-CBPP_Healthy Michigan Plan Extension Letter