Blog
-
Preventive Services at Risk: Federal Instability and State Responses
In late June, the Supreme Court upheld the Affordable Care Act’s (ACA) preventive services provision, preserving—for now—zero cost sharing access to screenings, vaccines, and other preventive care for more than 150 million people. The decision in Kennedy v. Braidwood Management Inc. foreclosed a constitutional challenge to coverage of preventive care while underscoring new risks to consumers’ access to…
-
Unpacking the Rural Health Transformation Fund Created by Congress to Soften Impact of Medicaid Cuts on Rural Hospitals
I grew up in North Carolina and often split my time between the urban center of the state and some of its most beautiful and rural areas on the back sounds “Down East.” This part of NC is so rural and was isolated for so long, generations of residents still speak with a distinctive Elizabethan…
-
Medicaid Cuts Kick in Quickly and Quietly in Idaho
Amber and Darrell Daniels with three of their four children. They live in Caldwell, Idaho. Darrell works for a pest control company while Amber enjoys being a stay-at-home mom to care for their children
-
Progress for Children is Eroding as Child Uninsured Rate Spikes to Highest Level since 2014
Every year we examine data provided by the U.S. Census Bureau’s American Community Survey (ACS) which provides the most comprehensive look nationally and by state at important trends impacting America’s families – including health insurance. Today we are sharing our analysis of data that came out just yesterday for calendar year 2024. Our analysis is…
-
Who Cares for Our Nation’s Children? Federal Medicaid Cuts Will Magnify Challenges for Child Care Workforce and the Young Families They Support
Last spring we walked through Medicaid’s role in supporting early childhood educators and subsequently the risks of proposed federal Medicaid cuts to the child care system. Fast forward to July 4th: the HR 1 “Megabill” was rushed through reconciliation and signed into law, leading to the biggest cut in Medicaid’s 60-year history. These cuts– and…
-
What does the CDC’s Vaccine Panel have to do with Medicaid?
Vaccine safety and changes happening at the Department of Health and Human Services (HHS) have been an ongoing topic of conversation throughout the past few months. As we have previously discussed here on Say Ahhh!, HHS has announced upcoming studies and potential changes to how vaccines are approved and recommended for different populations. Most notably,…
-
US Uninsured Rate Stays Level in 2024 for Adults and Kids: Storm Clouds Lie Ahead
Today the U.S. Census Bureau released the Current Population Survey (CPS) for 2024 which examines income, health insurance and other trends. Overall, the uninsured rate was unchanged at 8%; the child uninsured rate was 6.1%. – a slight increase that was not statistically significant. Later this week we will get state by state data from…
-
What is the Current Status of Vaccines in the US?
As fall respiratory virus season ramps up, major changes to the vaccine policy landscape in the U.S. are coming. Some states, such as Florida, have announced an effort to end all vaccine requirements for children to attend school. Federally, changes promulgated by the Secretary of Health and Human Services (HHS), Robert F. Kennedy Jr., have…
-
Federal Threats to Maternal and Infant Health Highlighted in Health Affairs
A recent article in Health Affairs Forefront argues that threats to policies, programs, and data systems will substantially set back progress made over the past few years in addressing the maternal and infant mortality. As a group of experts who previously served as federally-appointed members of the US Department of Health and Human Services (HHS)…
-
How Will We Know if States are Ready to Implement HR 1 and Work Reporting Requirements? Follow the State Performance Metrics Here.
States are just emerging from the unwinding of the pandemic-related Medicaid continuous enrollment provision when HR 1 presents a host of state budget impacts and new administrative hurdles for states. If states are already having trouble keeping up with their eligibility and enrollment administrative workload, adding work reporting requirements, six-month renewals, and mandatory cost sharing…
-
Untangling the Current Debate Around Federal Medicaid Cuts, the “Rural Health Transformation Program” and State Medicaid Budgets
The Congressional Budget Office estimates that the budget reconciliation law signed into law by President Trump (HR1) will result in a gross reduction of $990 billion in federal Medicaid/CHIP spending over 10 years and an increase in the number of uninsured Americans by 10 million. This is the largest cut to Medicaid in the history…
-
What to Expect From This Year’s Census Data on Child Health Coverage Rates: Will it be the Big Reveal on the Impact of Medicaid Unwinding?
As we wait for the annual September release of key Census Bureau data on health insurance status, what are we at CCF expecting with respect to children? The data covers 2024, a year in which most states finished the process of Medicaid “unwinding” – a multi-year process during which everyone on Medicaid had their eligibility…
-
Medicaid Work Reporting Requirements: Feds Forcing States to Spend Resources to Cover Fewer People
As discussed in our overview of H.R. 1, the budget reconciliation bill passed by Congress and signed by President Trump, the new law includes a harmful new work reporting requirement for Medicaid. The Congressional Budget Office estimates this work reporting requirement will result in a $326 billion cut in federal funding for states and lead…
-
New Resource on State-by-State Impacts of Budget Reconciliation Law
On July 4, 2025, President Trump signed the Congressionally-passed budget reconciliation law, known as “One Big Beautiful Bill,” into law. As we have talked about extensively, this law will drastically cut federal funding for Medicaid and hamstring states’ ability to fund their portion of the federal-state partnership. Many of the law’s provisions target Medicaid expansion…
-
Medicaid Managed Care: The Big Five in Q2 2025
Q2 2025, which ended on June 30, is not just another quarter. That’s because on July 4 the Budget Reconciliation Law (P.L. 119-21) was signed into law. That law makes major cuts to Medicaid, reducing federal payments to states by $990 billion over the next ten years and leaving 7.5 million Americans uninsured in 2034.…
-
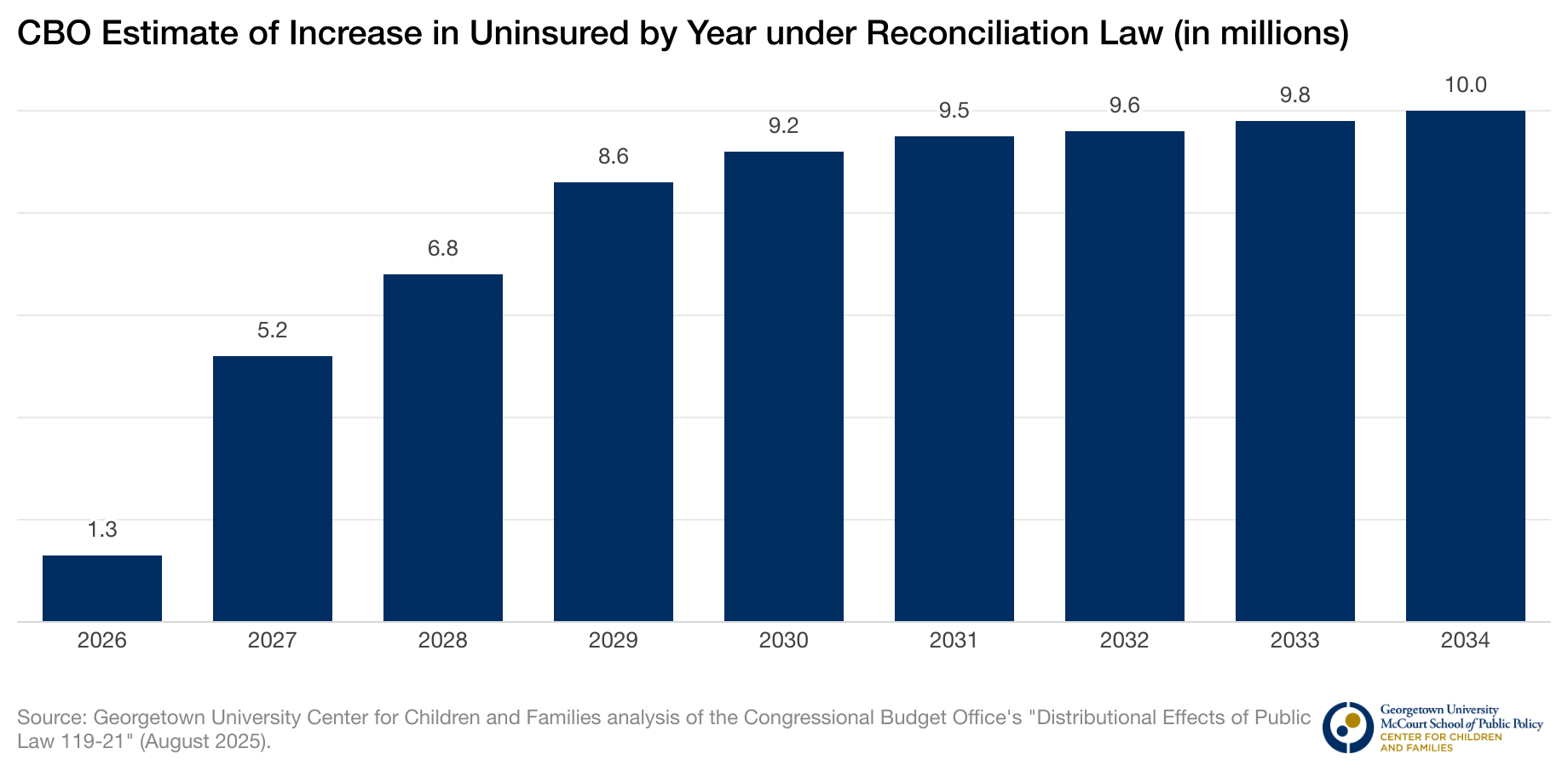
New CBO Health Coverage Estimates of Budget Reconciliation Law
On August 11, 2025, the Congressional Budget Office (CBO) issued more detailed estimates of the impact of the budget reconciliation law (H.R. 1 or P.L. 119-21) on health coverage. Consistent with final cost estimates issued in July, CBO finds that the reconciliation law will increase the number of uninsured people by 10 million in 2034, relative…
-
What to Expect From States When They’re Expecting Big Changes Due to HR 1
The passage of the recently enacted tax and budget law (HR1) will have major implications for state budgets, but the impact will be disproportionate. For example, Medicaid, expansion states (plus Wisconsin and Georgia) will be required to implement work requirements, increasing administrative costs while putting up barriers to enrollment and retention. Other states will be…
-
Trump Administration Blocks States from Keeping Babies and Toddlers Connected to Health Coverage
On Sunday, the Administrator of the federal Centers for Medicare and Medicaid Services (CMS), Dr. Mehmet Oz, appeared on Face the Nation. He was pressed repeatedly on Medicaid cuts by Host Margaret Brennan and responded by emphasizing the need for Medicaid to protect young children, paraphrasing the late Senator Hubert Humphrey in noting that any…
-
New Federal Budget Law Spells Trouble for Patients with Insulin-Requiring Diabetes
By: Billy Dering, Amy Killelea, and Christine Monahan (Georgetown University Center on Health Insurance Reforms) The recently enacted federal budget law is set to significantly roll back critical provisions of the Affordable Care Act (ACA) that have expanded health insurance coverage to millions. The law takes aim at health care programs that primarily serve low- and moderate-…
-
Fraud and Abuse Against Medicaid: The Truth About the Budget Reconciliation Law
After the House passed its version of what was then known as the “One Big Beautiful Bill Act,” we examined Speaker Johnson’s assertion that the House had not cut Medicaid but had instead targeted waste, fraud, and abuse in the program. We reported that just seven of the 24 Medicaid provisions in the bill truly…