Blog
-
Executive Director Joan Alker sits down with Georgetown University Provost Bob Groves
Executive Director Joan Alker recently sat down with Georgetown University Provost Bob Groves to discuss the history of the Center for Children and Families, and how our work has grown and adapted to expand and improve access to high-quality health care for our nation’s children and families. Listen now to hear more about our mission,…
-
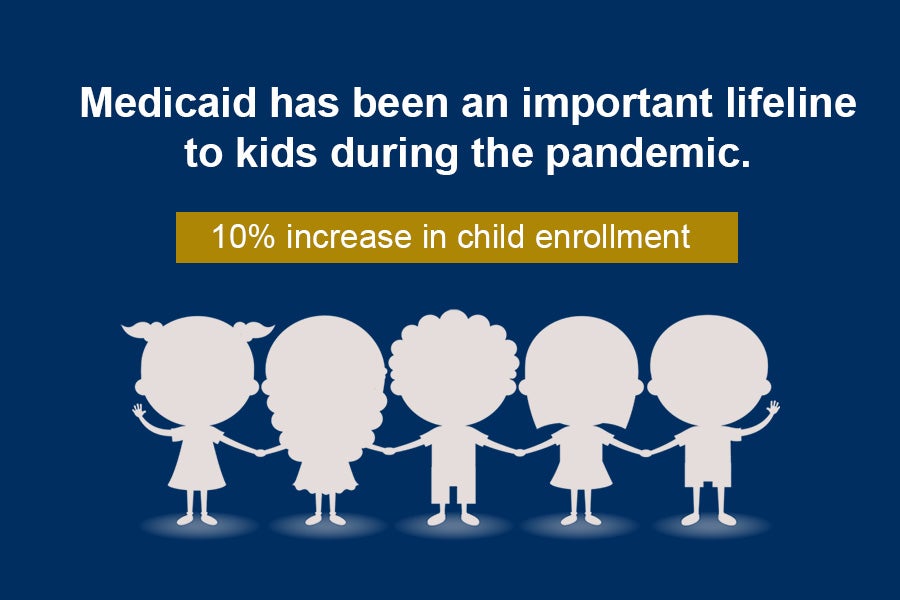
Child Medicaid Enrollment Grew by 10% during the Pandemic in 2020
The chair of the Federal Reserve, Jerome Powell, recently explained that the official unemployment statistics are too low, and that unemployment was closer to 10% in January. With the pandemic still raging and economic conditions looking very troubling, Congress is considering a COVID relief package with some important Medicaid provisions – my colleague Edwin Park…
-
House Energy and Commerce Committee Reconciliation Legislation Would Spur Medicaid Expansion and Promote Maternal Health
The House Energy and Commerce Committee has unveiled its portion of the House COVID-19 relief reconciliation bill, with a markup of the Committee’s recommendations scheduled for Thursday, February 11, 2021. Several of the Energy and Commerce Committee’s reconciliation provisions strengthen Medicaid and the Children’s Health Insurance Program (CHIP), including provisions to encourage states to finally…
-
House Energy and Commerce Committee Reconciliation Legislation Includes Sound Medicaid Drug Rebate Provision
Last night, the House Energy and Commerce Committee unveiled its recommendations for the House COVID-19 relief reconciliation bill, with a markup scheduled for February 11, 2021. One sound Medicaid provision would, as of January 1, 2023, eliminate the current cap on total drug rebates that manufacturers must pay state Medicaid programs, which would produce significant…
-
President Biden’s Executive Order on Public Charge
On February 2, 2021, President Biden issued an Executive Order (EO) on various aspects of the U.S. immigration system, including public charge policies. Readers of SayAhhh! know that the Trump Administration changed longstanding public charge policies to make it harder for lawfully residing immigrants to obtain green cards by imposing a new wealth test. Though…
-
Trump’s Farewell Gift to Florida’s Medicaid Program
A few days before departing, former CMS Administrator and Trump appointee Seema Verma handed out ten-year Medicaid demonstration waiver extensions for political allies, with Texas and Florida,[1] approvals being granted late Friday, January 15th. The Friday before (Jan. 8th) CMS had approved the infamous and dangerous Tennessee waiver, which my colleagues explained beautifully here. Ten…
-
Assessing the Trump Administration’s Final Medicaid Drug Rebate Rule Changing Best Price Reporting under Value-Based Purchasing Arrangements
On December 31, 2020, the Trump Administration finalized a rule that among other provisions, newly allowed drug manufacturers to report a range of prices offered through value-based purchasing arrangements (VBP) under the “best price” requirement under the highly effective Medicaid Drug Rebate Program (MDRP). This final rule from the Centers for Medicare and Medicaid Services…
-
Improving Medicaid Managed Care for Children: What a Dashboard Could Do
This is the season of Medicaid policy options—especially those competing for the attention of a new Administration and a new Congress. But the federal government is not the only audience; this week a terrific report was issued to policymakers in California. Written by Jocelyn Guyer (a former CCFer), Alice Lam, and Madeleine Toups at Manatt…
-
A Check-In on Leveraging the Power of Children’s Check-Ups
By Donna Cohen Ross, Jocelyn Guyer, Alice Lam and Madeleine Toups The pediatric primary care setting provides a near-universal opportunity to support the youngest patients and their caregivers, strengthening vitally important foundational relationships and promoting social and emotional development. When it launched in 2017, the Pediatrics Supporting Parents (PSP) initiative set out to explore core practices…
-
MACPAC Recommends One Year of Postpartum Medicaid Coverage at 100% Match
The momentum for extending postpartum Medicaid and CHIP coverage accelerated last week, with the Medicaid and CHIP Payment and Access Commission (MACPAC) giving a strong endorsement of the policy. MACPAC voted to recommend that Congress act to guarantee 12 months of postpartum coverage for pregnant individuals in Medicaid, and to align the policy in states…
-
Groups Call on HHS to Cut Red-Tape and Remove Barriers to Medicaid Coverage
A total of 116 organizations led by Georgetown University CCF and the Center on Budget and Policy Priorities sent a letter to the Acting Secretary of HHS urging immediate action to protect people who rely on Medicaid for their health insurance and who live in states with proposed or approved section 1115 work and community…
-
Medicaid Wars: The Unwinding Begins (Episode I)
Over the past four years, the Trump Administration has tried to undermine Medicaid by capping federal funding and stigmatizing its beneficiaries. This relentless ideological assault continued to the bitter end, even after the January 6 attack on the Capitol. As my colleague Joan Alker has explained, Secretary Azar and CMS Administrator Verma took actions on…
-
Biden Administration Announces It Will Reopen Federal Marketplace Enrollment
Today, January 28, 2021, President Biden signed an executive order establishing a new special enrollment period for the Affordable Care Act’s marketplaces in most states, in order to increase health coverage during the COVID-19 pandemic. The special enrollment period will begin February 15, 2021 and run through May 15, 2021 and like the annual open…
-
Senate Voting Rules and Budget Reconciliation Explained (Part 2)
In part 1 of this budget reconciliation refresher, I wrote about the basic rules for passing legislation in the House versus the Senate and how the budget reconciliation process allows certain legislation to move forward with approval from a simple majority of Senators rather than the usual three-fifths or 60-vote threshold. Now I’d like to…
-
Senate Voting Rules and Budget Reconciliation Explained (Part 1)
In the House of Representatives, legislation passes with a simple majority of 218 of 435 votes recorded on an electronic voting system. The Senate system is, by comparison, stuck in the dark ages. In the Senate, the clerk calls the names of each Senator and records the votes on a tally sheet. Like the House,…
-
Biden Administration Promises Predictability on Future Extensions of the Public Health Emergency
In a recent letter to Governors, Acting Health and Human Services Secretary Norris Cochran signaled that the COVID-19 public health emergency (PHE) “will likely remain in place for the entirety of 2021.” Moreover, the letter assures states that when a determination is made to terminate the PHE or let it expire, HHS will provide states…
-
Critical Health Equity Context Needed in New Maternal and Infant Health Data Profile
Just before the end of 2020, CMS published a valuable new trove of data on indicators of maternal and infant health in Medicaid, designed to create a profile of the health status of pregnant and postpartum women and their infants. The information is part of several new reports and learning communities launched by CMS to…
-
The Tennessee Waiver: Block Grant, Aggregate Cap, or Windfall?
In their wondrous 1957 interpretation of a Gershwin classic, Ella Fitzgerald and Louis Armstrong sing, “You like potato and I like potahto/You like tomato and I like tomahto.” Their back-and-forth has echoes in the current debate over what to call the TennCare III demonstration, approved on January 8 by the former CMS Administrator, Seema Verma.…
-
Another Parting Gift for the Biden Administration – the “SUNSET” Rule
The great American singer Wilson Pickett probably was not thinking of the SUNSET rule when he wrote his soul anthem, “In the Midnight Hour.” But Secretary Azar waited ‘til the midnight hour, and there it is, in the January 19, 2021 Federal Register: “Securing Updated and Necessary Statutory Evaluations Timely,” a final rule issued by…
-
Trump Administration Tries Its Best to Knock Legs Out from Under Medicaid on the Way Out the Door
So far 2021 has been a really wild and difficult ride for me and millions of others in the U.S. with COVID-19 ravaging the nation, an armed insurrection here in DC, and an ongoing economic crisis leaving so many families in need. My mind has been struggling to absorb all that is happening so quickly.…