Managed Care
-
Medicaid Managed Care: The Big Five in PHE Q10 (Q2 2022)
June 30 marked the end of calendar quarter 10 of the COVID-19 Public Health Emergency (PHE), or PHE Q10. For the five national companies with the largest Medicaid managed care businesses, the past two- and one-half years have been a period of particularly robust growth. Since PHE Q1, which ended on March 31, 2020, enrollment…
-
Bipartisan Safer Communities Act Provision Directs CMS to Review State EPSDT Implementation, including in Managed Care
Last month my colleague Anne Dwyer summarized the now-enacted Bipartisan Safer Communities Act and its provisions with potential to boost access to mental health services for children and families. One we will be watching closely: a review of state Medicaid EPSDT requirements, services, and practices. Long time Say Ahhh! Readers know that Medicaid’s Early Periodic…
-
Transparency in Medicaid Managed Care: Are the Times A-Changin’?
If the phrase “transparency in Medicaid managed care” sounds like an oxymoron, that’s because in many states it is. Finding information on the performance of individual Medicaid managed care organizations (MCOs) for children and families and other Medicaid beneficiaries on state Medicaid agency websites can be challenging. This is more than unfortunate because in the…
-
An Advocate’s Guide to Medicaid Managed Care Procurement
2022 is a big year for Medicaid managed care procurements. Procurements are already underway in California, Iowa, and Nebraska with awards scheduled to be announced in August. New Mexico is scheduled to launch its procurement in September, and three more states — Florida, Georgia, and Texas — are expected to issue Requests for Proposals (RFPs)…
-
A Guide for Health Care Advocates: Medicaid Managed Care Procurement
Overview Most Medicaid beneficiaries in most states are enrolled in managed care organizations (MCOs). (See text box, “What’s a Medicaid MCO?”) State Medicaid agencies contract with MCOs to assemble networks of health care providers to furnish services to program beneficiaries and protect them from medical debt. Simply put, if an MCO does not do its job,…
-
Take the Child Health Dashboard Tour
Since we debuted the Dashboard Library, we’ve been keeping our eyes on state Medicaid agency websites and are pleased to announce that we’ve discovered quite a few more. The dashboards we’ve added to the list vary widely in content and presentation style, ranging from slides to interactive workbooks. Unfortunately, none of the dashboards that we…
-
Show Me the Data: A Medicaid Dashboard for Missouri
We are pleased to announce the most recent addition to our library of Medicaid dashboards: Missouri. One of the most important functions of easily accessible and digestible data (like a dashboard) is the increased transparency that it offers both Medicaid beneficiaries and advocates. This is especially significant when it comes to holding Managed Care Organizations…
-
Standards for Provider Network Adequacy in Medicaid and the Marketplaces
The Centers for Medicare & Medicaid Services (CMS) has issued final rules for provider network adequacy in Qualified Health Plans (QHPs) offering coverage in the Marketplaces that the federal government operates through HealthCare.gov. Under these rules, which come with the snappy title, “Notice of Benefit and Payment Parameters” and the even snappier initialism (NBPP), CMS…
-
Medicaid Managed Care: The Big Five in PHE Q9 (Q1 2022)
March 31 marked the end of the ninth quarter of the COVID-19 Public Health Emergency (PHE). First declared by the Secretary of HHS on January 31, 2020, the PHE has subsequently been extended nine times, through July 15. As long as the PHE is in place, states qualify for an additional 6.2 percentage points on…
-
New Florida Law Requires Stratified Performance Measure Data for Medicaid Managed Care
By Anne Swerlick, Senior Policy Analyst, Florida Policy Institute Experts agree that to reduce health disparities, you first need to know where they exist. The collection of health plan performance measure data, such as timely prenatal care and well-child check-ups, broken down by demographic factors like race and ethnicity is essential for developing targeted health…
-
Medicaid Managed Care Compliance Tools: Another ‘Pay-For’
Discussions have begun on the possibility of enacting a scaled-down version of the Build Back Better legislation. Any agreement that includes new federal spending will also require pay-fors (a/k/a offsets) either in the form of spending reductions or tax increases, or both. In Medicaid, responsible pay-fors—i.e., policy changes that the Congressional Budget Office will score…
-
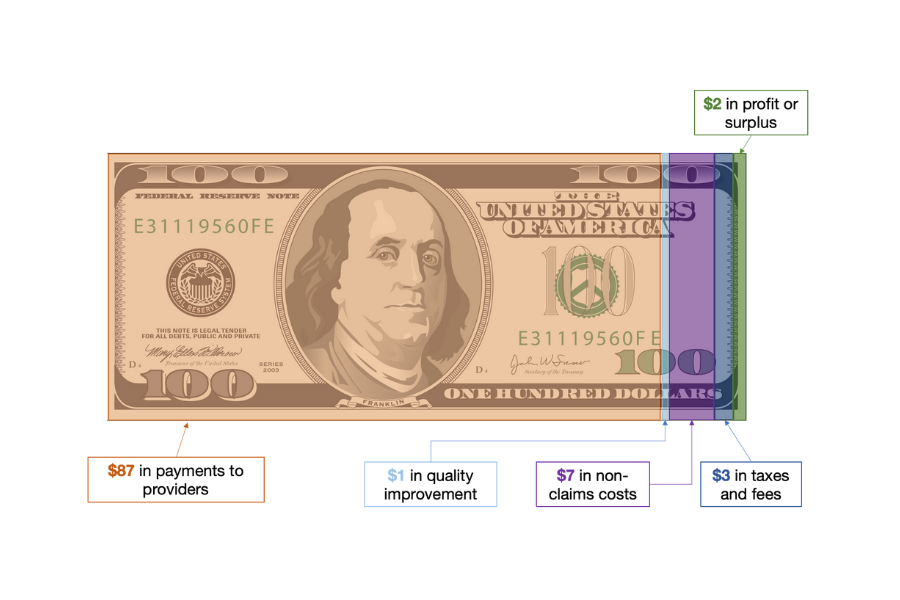
Medicaid Managed Care: SDOH, MCO, and MLR
There is no shortage of acronyms or initialisms in government agencies and programs and Medicaid is no exception. The Medicaid and CHIP Payment and Access Commission or MACPAC (one of our favorite acronyms) devotes an entire glossary to them. The most prominent initialism in Medicaid policy discussions these days is SDOH: social determinants of health,…
-
Medicaid Managed Care: What Can the Annual MLR Report Tell Us?
Over 32.8 million children are covered by Medicaid, and the large majority are enrolled by their state Medicaid agencies in managed care organizations (MCOs). In exchange for monthly capitation payments, the MCOs contract with the state Medicaid agency to furnish covered services through networks of providers. These arrangements, in 40 states and the District of…
-
California’s Medicaid Managed Care Procurement: A Leap Forward
Last week, California’s Medicaid agency issued a Request for Proposals (RFP) to provide managed health care services to program beneficiaries. This is not just another Medicaid RFP. California is far and away the nation’s largest Medicaid managed care market. As of September 2021 the state Medicaid agency contracted with 24 managed care organizations (MCOs) to…
-
Medicaid Managed Care Financial Results for 2021: A Big Year for the Big Five
The Q4 2021 earnings reports are in, and the five largest companies in the Medicaid managed care market—CVS Health, Anthem, Centene, Molina, and UnitedHealth Group—did very well, thank you very much. CVS Health made $17.3 billion last year; Anthem, $7.5 billion; Centene, $1.8 billion; Molina, $1.0 billion; and UnitedHealth Group $24.0 billion. Not all of…
-
California’s Medicaid Managed Care Waiver: New Potential for Access and Transparency
One of the most significant Medicaid managed care developments in 2021 happened on December 29, when CMS approved federal funding and waivers for California’s reform initiative, Advancing Innovation in Medi-Cal (CalAIM). The approval involved two sets of waivers, one operating under section 1115 of the Social Security Act, the other under section 1915(b)(4). For good…
-
Medicaid Managed Care in 2021: The Year that Was
The Medicaid managed care ecosystem is huge and complex. (If you need a primer, the health policy podcast Tradeoffs has a short and entertaining one). As of March of this year, forty states and the District of Columbia were contracting with over 280 different managed care organizations (MCOs). The federal government and states combined spend…
-
CMS Tools Suggest Key Roles for Managed Care Plans in Helping Enrollees Retain Coverage
While we were all unwinding from our Thanksgiving celebrations, CMS was busy putting out two new tools to assist state Medicaid eligibility and enrollment operations. The first is focused on preparing for the return to normal operations after the COVID-related continuous enrollment requirement is lifted while the second is a refresher on best practices and…
-
Medicaid Managed Care: Results for the “Big Five” in Q3
The Q3 results for the “Big Five” are in. Loyal readers of the Say Ahhh! Blog will recognize them as the publicly-traded companies with the largest shares of the Medicaid managed care market: Aetna/CVS, Anthem, Centene, Molina, and UnitedHealth Group. Their Medicaid footprints for the quarter ending September 30, summarized below, reflect a continuation of…