Medicaid
-
Cuts to Medicaid Expansion in the Proposed Budget Reconciliation Bill being Considered by Congress
FMAP Cuts Tied to State Decisions to Expand Comprehensive Health Coverage with State-Only Funds to Children Regardless of Immigration Status Section 44111 of the proposed budget reconciliation bill being marked up by the House Energy and Commerce Committee today targets the Affordable Care Act’s Medicaid expansion for cuts with an apparent aim to advance a…
-
How Do We Know Congress’s Work Requirements in Medicaid Will Fail? They Already Have.
As expected, the House’s rushed attempt to finance the Trump Administration’s immigration and tax agenda by cutting Medicaid includes a “work requirement.” Proponents claim that it is intended to support employment but it does no such thing. In fact, it’s a policy that takes health insurance away from millions of people, including workers. This policy…
-
House Energy and Commerce Committee Medicaid Provisions Released, Mark-Up Set for Tuesday
Statement by Joan Alker, Executive Director of the Georgetown University Center for Children and Families, regarding Medicaid provisions included in the House Energy and Commerce budget reconciliation bill text scheduled for mark-up this week “The House Energy and Commerce Committee released the text of its portion of the reconciliation bill at around 10 p.m. last…
-
CCF Marks 20th Anniversary as Ominous Cuts to Medicaid Loom
The Center for Children and Families turned 20 on Monday! I marked this milestone as a guest on the NPR 1A program, explaining the role of Medicaid and Congressional proposals to cut it deeply. Many of the listeners needed no convincing that Medicaid was important, indeed life-sustaining for them and their families. One mother called…
-
Research Update: Estimates of State Impact of Medicaid Cuts
As we have written about extensively on Say Ahhh!, Medicaid is facing large cuts in the budget reconciliation process with hundreds of billions of dollars on the chopping block. It’s unclear how policymakers will meet the hundreds of billions in cuts assigned to programs under the jurisdiction of the House Energy and Commerce Committee but…
-
How Medicaid Supports Older Adults
In Partnership with: Most people are familiar with Medicare as a major source of health coverage for seniors. However, Medicaid also provides crucial coverage for millions of older adults. Over 7 million seniors age 65 and up, including 4.2 million older adults of color, rely on Medicaid to access long-term care and make Medicare more…
-
Rescinding the Eligibility and Enrollment Rule Would Thwart Efforts to Improve Efficiency in Medicaid and Efforts to Reduce Improper Payments
Congressional leaders have repeatedly said they are going to protect the most vulnerable from a loss of Medicaid coverage and focus on addressing “waste, fraud, and abuse” but rescinding the Eligibility and Enrollment rule would do neither. The Eligibility and Enrollment Rule (E&E rule) finalized by the Biden Administration in April 2024 is on the…
-
Webinar: How Medicaid Supports the Child Care Workforce
The Georgetown University Center for Children and Families, National Association for the Education of Young Children, and Center for Law and Social Policy held a webinar on Thursday, May 1st at 3 pm ET. The role of Medicaid: Because child care is a historically underinvested system, many child care centers are unable to provide their…
-
Federal Medicaid Cuts Would Harm State GDP, Credit Ratings, Jobs and Health Systems
Medicaid is the nation’s largest health insurer, providing over 70 million children, parents, people with disabilities, and low-income seniors with health coverage. It’s clear that the major cuts to Medicaid funding currently under consideration in Congress would impact the health care system as a whole – health providers would have fewer insured patients, lower payment…
-
Thinking Frequent Medicaid Redeterminations Won’t Hurt Children’s Health Insurance? Take a look at What Happened in Texas.
Nearly half (47%) of the 79 million people who get their health insurance through Medicaid are children. To ensure continuity of coverage for children, Congress took action to protect children’s access to health insurance by requiring states to provide a full year of continuous coverage in Medicaid to children beginning in 2024. But will children’s…
-
Combined Impact of Medicaid Cuts Under Consideration Would End Expansion and Take Away Coverage for Nearly 21 Million Low-Income People
In analyzing the draconian Medicaid cuts under consideration by House Republicans for inclusion in budget reconciliation legislation, it is often easier to examine each specific proposal in isolation. But it is important to also take a step back and look at how these proposals would interact with each other. In doing so, it is virtually…
-
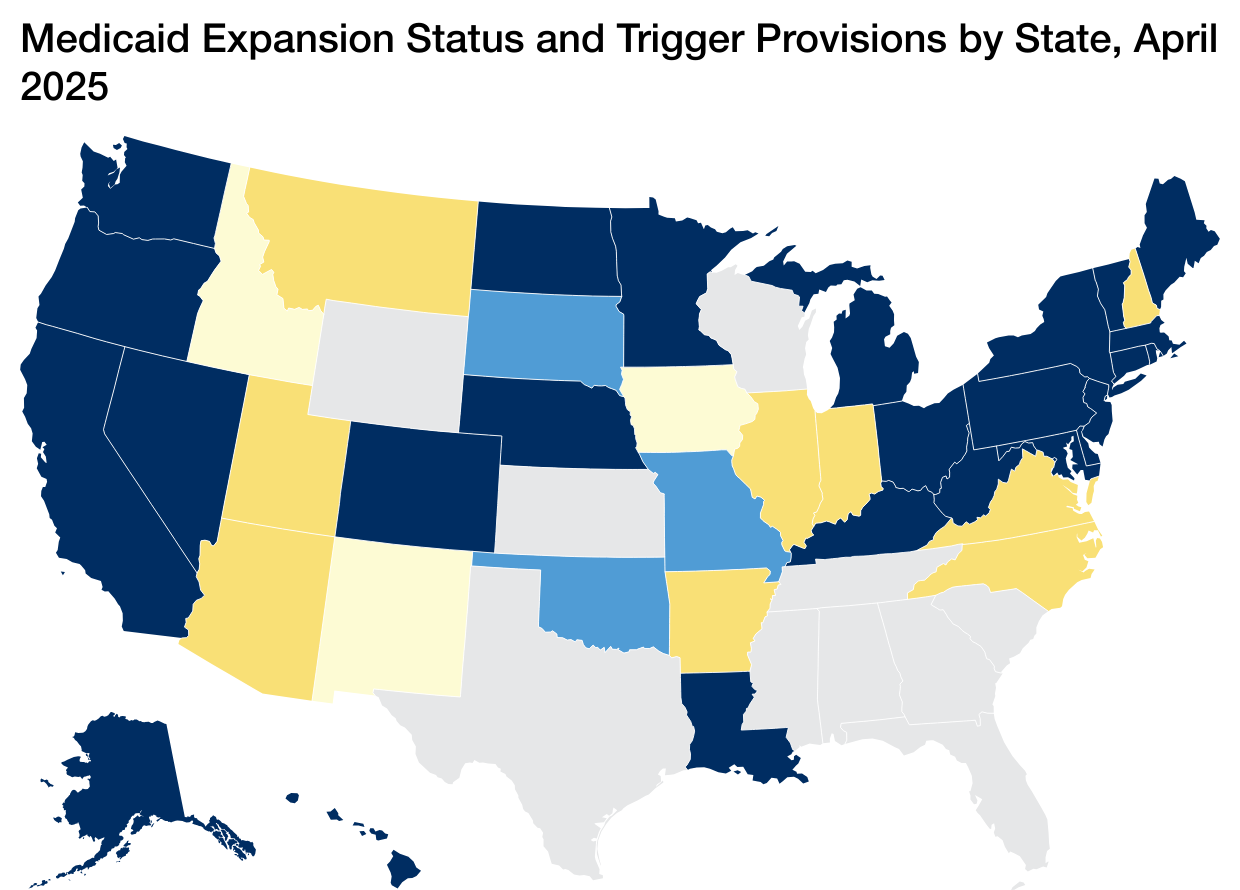
How Would Changes to Federal Medicaid Expansion Funding Impact People in “Trigger” States and Those with Expansion Enshrined in State Constitutions?
Congress is currently considering draconian cuts to Medicaid that would mean millions of low-income Americans lose access to affordable health care. But both the type of federal cuts and how the joint state-federal Medicaid program operates in each state mean that the impact on people living in different states would vary considerably. The major difference…
-
Medicaid Work Reporting Requirements – Even with Exemptions – Will Have Significant Consequences for People with Substance Use Disorders
As highlighted on Say Ahhh! earlier this month, Congress continues to consider imposing work reporting requirements on people who get their health coverage through Medicaid. As a practical matter, one thing is clear: the only purpose of this proposal is to terminate Medicaid coverage for the most vulnerable Americans. Work reporting requirements in public benefit…
-
Cuts to ACA’s Medicaid Expansion Under Consideration by Congress would Lead to Large Coverage Losses Hitting some States Harder than Others
Next week, the House Energy and Commerce Committee is expected to consider fast-track budget reconciliation legislation that could cut Medicaid by as much as $880 billion over 10 years or more. This level of cuts to Medicaid is unprecedented and if enacted would mean tens of millions of children, parents, seniors, people with disabilities and…
-
New State-by-State Estimates of the Federal Funding Cuts from Imposing a Per Capita Cap on the Medicaid Expansion
I previously warned about how imposing a per capita cap on the Medicaid expansion would effectively lead to a sharp cut to the current 90 percent matching rate for the 40 states and the District of Columbia that have adopted the expansion. This would shift significant costs to states, force them to drop their expansions…
-
Governors and State Agencies Estimate Impact of Potential Federal Medicaid Cuts on State Budgets
With Congress returning to DC, we expect to learn more about the Medicaid cuts under serious consideration as part of the budget reconciliation process fairly soon. But, in the meantime, states are starting to crunch some numbers to gauge the impact of the potential Medicaid cuts on their state programs and state budgets. The analysts…
-
The U.S. Already Has a Child Care Crisis: Medicaid Cuts Would Make it Much Worse
Working parents don’t need survey data to tell them our nation is facing a serious child care crisis. They are reminded every time they pay their child care bill that often exceeds even the high cost of rent. Expectant parents learn about it when they add their names to long waitlists even before their child…
-
Child Medicaid Policy Institute Webinars
The Georgetown University Center for Children and Families’ new Child Medicaid Policy Institute (CMPI) seeks to educate child health advocates, providers, other stakeholders, and policymakers on the fundamentals of the Medicaid program and its importance for children, families, and other low-income individuals. Starting in December 2024, CMPI has hosted a series of public webinars on…
-
Webinar: Medicaid Provider Taxes: How States Use Them and Budgetary Effects of Proposed Federal Changes
The Georgetown University Center for Children and Families invites you to a special session of our new Child Medicaid Policy Institute (CMPI) on Wednesday, April 23rd, at 3:00pm ET. This webinar is free and open to the public. CMPI is excited to host another webinar on a relevant topic: Medicaid provider taxes. In the current debate on the federal budget…
-
Medicaid is a Critical Support for the Early Childhood Education Workforce
In Partnership with Medicaid is an important source of health coverage for the early childhood education professionals who support child development and care for children while parents work, and for the children and families these educators serve. At least thirteen states cover more than a third of the child care workforce through Medicaid, making the…