Medicaid
-
Medicaid Managed Care Transparency: What Can Quality Data Do?
Earlier this week the data transparency door to Medicaid managed care opened. Not as wide as some of us would hope, but wide enough to start a detailed conversation about the performance of individual MCOs on quality. It happened at a briefing sponsored by the California Health Care Foundation and took the form of a…
-
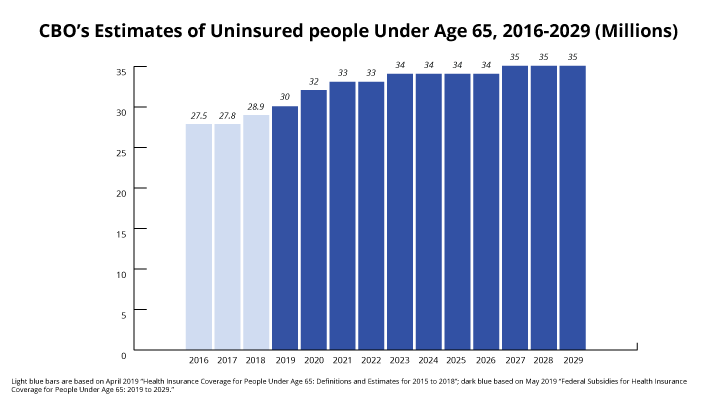
New CBO Baseline Expects Number of Uninsured to Rise by 5 Million Over Next Decade
On May 2, the Congressional Budget Office issued its new baseline, including health coverage projections for the period 2019-2029. CBO expects the number of non-elderly uninsured people nationwide will increase by 5 million over the next ten years, from 30 million in calendar year 2019 to 35 million in calendar year 2029. That is in…
-
Pediatricians and CCF Release 2019 State Snapshots on Children’s Health Coverage
We’ve continued the tradition we started three years ago with our colleagues at the American Academy of Pediatrics to create state snapshots that focus on the valuable role Medicaid and CHIP fill for children. These snapshots provide details on who’s covered by Medicaid and CHIP in each state and how Medicaid/CHIP fit into the overall…
-
Why is Florida’s Medicaid Work Reporting Proposal the Harshest in the Country for Kids and Families?
A few weeks ago I blogged about Florida’s bill being the worst I have seen nationwide. The bill’s sponsor definitely didn’t read the blog (as was made clear during the House floor debate), nor did he seem concerned about the many valid criticisms raised during the debate, and the bill passed the House last week…
-
State Medicaid and CHIP Snapshots, 2019
The Georgetown University Center for Children and Families (CCF) and the American Academy of Pediatrics (AAP) created factsheets underscoring the importance of Medicaid in providing coverage for children in all 51 states (including the District of Columbia). Sources are available. Previous snapshots can be found here.
-
Nebraska Residents Will Have to Wait for Medicaid Expansion While Governor Puts More Obstacles in Path to Coverage
Writer George Orwell would love the Nebraska Governor’s complex plan to implement the simple expansion of Medicaid health coverage passed by Nebraska voters in 2018 that would help an estimated 95,000 of the state’s residents gain coverage. In Orwell’s book “1984”, the fictional state of Oceania asked citizens to accept opposing ideas as both being…
-
Medicaid and Early Childhood Home Visiting Collaboration: A Washington Perspective
Early in Washington’s Medicaid and early childhood home visiting collaboration, it was clear we needed a common understanding of home visiting services compared to home-based Medicaid services. As it happens, there are some significant differences! Although the Centers for Medicare and Medicaid Services (CMS) does not authorize home visiting models in their entirety, they do…
-
New Data Show Widespread Decline in Child Enrollment in Medicaid/CHIP Coverage in 2018
We’ve been anxiously awaiting the release of final Medicaid and CHIP enrollment data for 2018, which was expected to be posted almost a month ago. The wait is finally over but not our concerns about what’s happening. In the meantime, more stories about eligibility system issues in a handful of states and states conducting more…
-
Updated CBO Estimates Find Uninsured Increased by 1.4 Million Between 2016 and 2018
Recently, as part of materials explaining the new version of its health microsimulation model, the Congressional Budget Office issued updated estimates for the number of non-elderly people without health coverage over the past four years. According to the CBO estimates, the number of uninsured people under age 65 rose from 27.5 million in fiscal year…
-
How Medicaid and CHIP Can Support Student Success through Schools
Seventh in a series of briefs on the future of children’s health care coverage Summary Recognizing that a healthy student is a better student, education and health officials have begun working closely in the past few years to integrate their efforts. Recent changes to federal education law, new grant programs and revised Medicaid rules have…
-
Centene’s takeover of WellCare: What would it mean for kids and families covered by Medicaid?
On March 27, the Centene Corporation announced it would acquire WellCare Health Plans, Inc. in a cash and stock transaction valued at $17.3 billion. The transaction is subject to approval by the shareholders of both companies as well as state regulators. The companies “expect to complete the transaction in the first half of 2020.” For…
-
New Research Documents Health Benefits of Medicaid Expansion
We like to review the research here at CCF and that certainly goes for papers examining the effects of Medicaid expansion. I pulled together a quick overview of that research last year and recently my colleague, Lauren Roygardner, has highlighted an impressive study showing Medicaid expansion improves access to treatments for opioid addiction. The studies…
-
Louisiana Launches Pilot Work Promotion Program Instead of Punitive Work Reporting Requirements
Gov. John Bel Edwards in Louisiana should be commended. Not only did he fulfil a campaign promise to expand Medicaid to thousands of Louisianans, but now he has launched a positive work support pilot program for Medicaid beneficiaries. Positive work support initiatives illustrate there are better ways to assist Medicaid enrollees in improving their employment…
-
Who’s Minding the Store for Tennessee Children Relying on Medicaid and CHIP?
When I began my career as a children’s advocate in the 90s, Tennessee led the nation in the percentage of its children with health insurance. It was a proud moment for our poor Southern state that was brought about by the vision and political effectiveness of Democrat Governor Ned Ray McWhether and by the courage…
-
Where Does the Trump Administration’s Medicaid Waiver Policy Go Next?
Last week was a busy week with a federal court vacating both Arkansas and Kentucky’s Medicaid Section 1115 waivers on Wednesday and the Trump Administration approving Utah’s partial expansion waiver with a work requirement and an enrollment cap on Friday—but without the full expansion match. (Read more on Utah past and present). Given the immediate…
-
Affordable Care Act Back in the Spotlight: Build on its Progress or Scrap it Entirely
It is hard to find a starker example of the different approaches our two political parties take to health care than the events of March 26, 2019. The day started with headlines about the Trump administration’s push to have the Affordable Care Act (ACA) declared unconstitutional, and ended with Democratic legislators in the U.S. House introducing a bill that…
-
When Early Childhood Educators are Covered, Kids Win: Stories from North Carolina
If you, like me, have the peace of mind of knowing that your toddler or preschooler is well cared for and supported while you’re at work, you probably know already that you’re incredibly fortunate. I am grateful every day for the many early childhood teachers who make the safety, educational success, and wellbeing of a…
-
Judge Blocks Arkansas and Kentucky Medicaid Work Requirement Waivers: What Does This Decision Mean for Other States?
Under the Administrative Procedures Act (APA), federal agencies may not take actions that are “arbitrary or capricious.” If they do, federal courts are instructed to hold the action unlawful and set it aside. Late yesterday afternoon, that’s exactly what Judge James E. Boasberg of the U.S. District Court in the District of Columbia did with…
-
Medicaid and CHIP Eligibility, Enrollment, and Cost Sharing Policies as of January 2019: Findings from a 50-State Survey
Executive Summary This 17th annual survey of the 50 states and the District of Columbia (DC) provides data on Medicaid and the Children’s Health Insurance Program (CHIP) eligibility, enrollment, renewal, and cost sharing policies as of January 2019. It is based on a telephone survey of state Medicaid and CHIP officials conducted by the Kaiser…
-
Hot Off the Press: Annual KFF 50-State Survey on Medicaid
This 17th annual KFF survey and key resource for Medicaid stakeholders reports eligibility, enrollment, renewal and cost-sharing policies in place as of January 2019 for children, pregnant women, parent/caretakers, and low-income adults in Medicaid and CHIP. Like the previous year, for the most part states continued to refine their efforts in delivering a streamlined, data-driven…