All
-
Medicaid Managed Care in 2023: The Year that Was
2023 marked an inflection point in the growth of Medicaid managed care. Enrollment in MCOs, which had climbed continuously in both 2021 and 2022 due largely to the continuous coverage policy in place during the Public Health Emergency, plateaued and then headed downward, due largely to the PHE unwinding. Much uncertainty remains as to how…
-
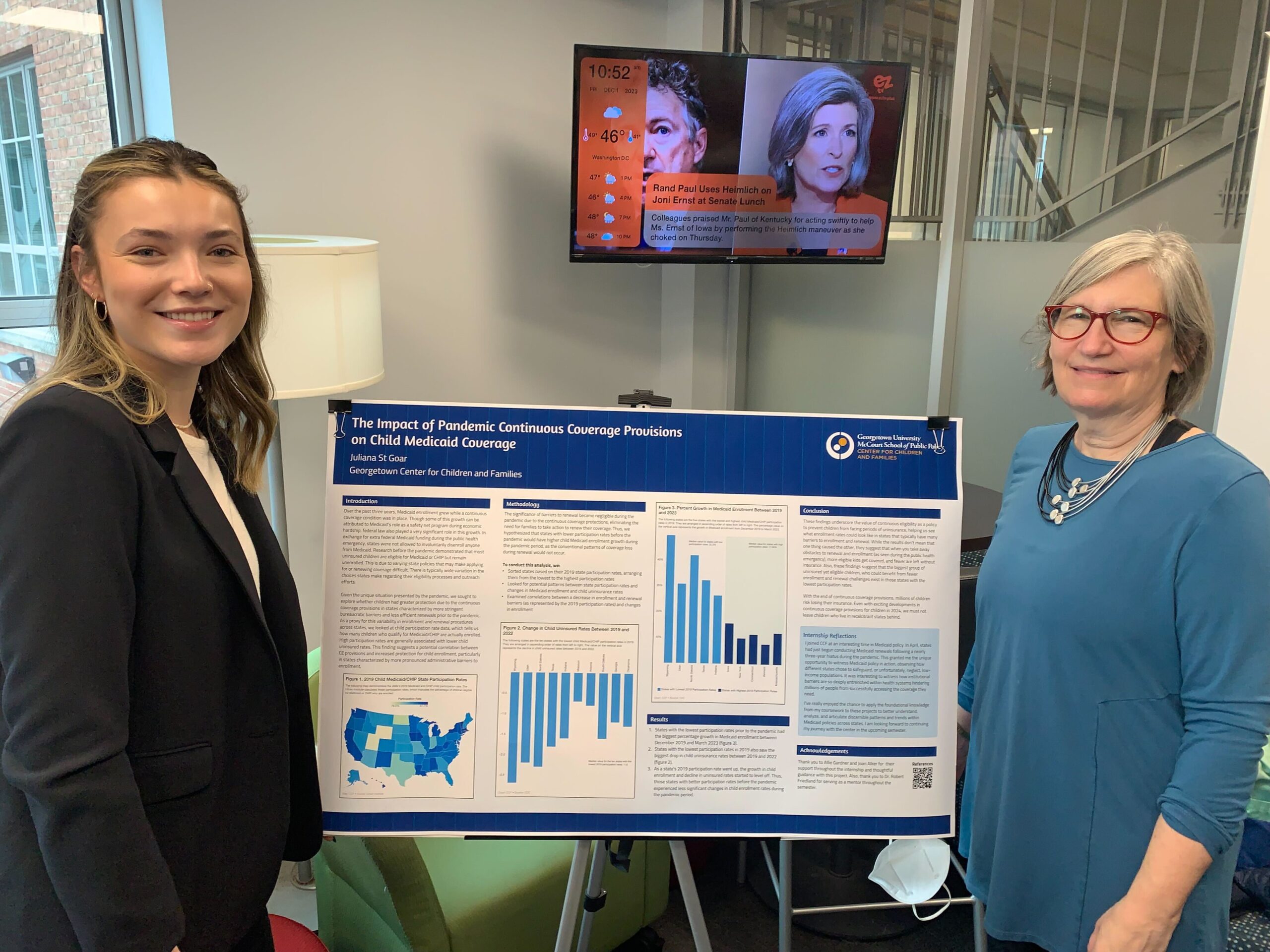
States with Low Medicaid Participation Rates Saw the Greatest Child Coverage Gains During the Period of Pandemic Continuous Coverage Protections
By: Juliana St Goar & Joan Alker It is well documented that over the past three years, Medicaid enrollment grew while a continuous coverage requirement was in place. Though some of this growth can be attributed to Medicaid’s crucial role as a safety net program during times of economic hardship, federal law also played a…
-
CCF Comments on Processes for Assessing Compliance with Mental Health Parity and Addiction Equity in Medicaid and CHIP
The Georgetown University Center for Children and Families submitted the following comments to CMS regarding the proposed processes for assessing compliance with mental health parity and addiction equity in Medicaid and CHIP. Read the Comments
-
Medicaid Expansion Enrollment Opens in North Carolina
On December 1, North Carolina became the latest state to expand Medicaid under the Affordable Care Act, meaning approximately 600,000 residents now have access to comprehensive health coverage. The North Carolina Department of Health and Human Services is now providing links and information on how to quickly apply for coverage either online, over the phone,…
-
In August, Marketplace Enrollment Slowed Among Those Losing Medicaid Coverage During Unwinding
As readers of Say Ahhh! know, I have been tracking monthly data (here, here, here, and here) from the Centers for Medicare and Medicaid Services (CMS) on the number of people who were either previously enrolled in Medicaid or had experienced a denial or termination who then selected a marketplace plan. CMS has just issued…
-
CMS Releases New Unwinding-Related Renewal Resources for Health Care Settings
CMS recently released a toolkit for clinical offices and health care settings with patient-centered messaging regarding the unwinding of the Medicaid continuous enrollment requirement. The toolkit includes helpful information on how health care providers can share information on Medicaid and CHIP renewals with patients. The toolkit starts with suggestions on what various staff members within…
-
Florida’s Rolling Out a New Medicaid/SNAP Portal Next Week – Throwing Gas on the Unwinding Fire
With little advance notice to the community, the state of Florida announced in mid-November that it was moving next week (December 5th) to a new portal for eligibility for Medicaid, SNAP, child care and TANF; and that every person/household in the state accessing those benefits will need to create a new account. Every person create…
-
Georgia Pathways Implementation: The Glass is 99.6% Empty
On October 5, 2023, CMS certified as complete Georgia’s implementation plan (the implementation plan itself starts on page 50) for phase one of its “Pathways to Coverage” section 1115 demonstration that the state had already started implementing more than 3 months earlier, on July 1, 2023. Yes, you read that right. And no, it doesn’t…
-
Biden Administration Says No to Premiums in Medicaid Again – This Time in Wisconsin
We’re getting to the end of the year and a seasonal tradition for Medicaid Section 1115 waiver watchers is observing an uptick in waiver activity by the federal Centers for Medicare and Medicaid Services (CMS). Last Friday, CMS issued a temporary one-year extension (in place until December 31, 2024) for Wisconsin’s BadgerCare Section 1115 demonstration…
-
Report Finds Child Uninsured Rate Improved in 2022, Warns Progress Under Threat as Eligible Children Lose Coverage During Medicaid Unwinding
This week we were joined by Stacey Pogue, a senior policy analyst with Every Texan and Dr. Valerie Borum Smith, a pediatrician and President-Elect of the Texas Society of Pediatricians to release our annual report on child health coverage trends. Our report showed the number of uninsured children declined in 2022 to one of the…
-
North Carolina and Hawaii Make 10: States Advancing Medicaid/CHIP Multi-Year Continuous Eligibility for Young Children
It’s hard to keep up with the rapid progress in the number of states seeking federal approval to adopt multi-year continuous coverage for children covered by Medicaid and the Children’s Health Insurance Program (CHIP). Since we last took stock, North Carolina and Hawaii have proposed 1115 waivers to adopt continuous eligibility for children from birth…
-
New CBO Study Explores the Long-Term Fiscal Benefits of Medicaid Coverage in Childhood
There is a large and growing body of research demonstrating the long-term benefits of Medicaid coverage during childhood and during pregnancy. This includes better health and lower incidence of disability in adulthood, higher educational attainment, and greater earnings and intergenerational mobility. Now, in a new working paper, the Congressional Budget Office (CBO) has conducted an…
-
Medicaid’s Pandemic-Era Continuous Coverage Protections Helped Reduce Number of Uninsured Children
Download Report PDF Introduction Data from the U.S. Census Bureau’s American Community Survey (ACS) for 2022 finds that the number of uninsured children continued to decline over the pandemic period – most likely as a consequence of the continuous coverage protection in Medicaid put in place by one of the first COVID-19 rescue packages, the…
-
Bipartisan Senate Finance Committee Legislation Includes Enhanced Medicaid Pharmacy Pricing Survey Provision
On November 8, 2023, on an unanimous 26-0 vote, the Senate Finance Committee approved the Better Mental Health Care, Lower-Cost Drugs, and Extenders Act. The bill includes a number of Medicare and Medicaid provisions but also incorporates two sound Medicaid drug pricing provisions related to “spread pricing” in Medicaid managed care and to Medicaid pharmacy…
-
Children’s Health Coverage Report 2023 Press Call
Listen to the Press Call Recording A new Georgetown University report with state-by-state data finds the child uninsured rate improved in 2022 due in large part to the federal Medicaid continuous coverage protection. This federal requirement ended in April and state Medicaid agencies started the unprecedented task of redetermining eligibility for all Medicaid enrollees, leading…
-
Can MMRCs Do More to Inform State Medicaid Maternal Health Efforts?
As rates of maternal mortality have risen in the United States, maternal mortality review committees (MMRCs) have been an important tool to understand why these maternal deaths occur. State MMRCs consist of multidisciplinary representatives to review deaths that occur during or within a year of pregnancy. In our recent 12-state scan of Medicaid MCO performance…
-
CCF’s Unwinding and Enrollment Trackers Explained
Since Medicaid unwinding of the continuous coverage requirement has begun, net child Medicaid enrollment has fallen by more than two million and overall net Medicaid enrollment has declined by more than five million. We have received some questions about how we calculate these net enrollment figures as well as the basis of other unwinding data…
-
Medicaid Managed Care: Results of the PHE Unwinding for the Big Five in Q3 2023
The “Big Five” Medicaid managed care companies—Centene, CVS Health (Aetna), Elevance Health (formerly Anthem), Molina Healthcare, and UnitedHealth Group—have reported their Medicaid enrollment for the quarter ending September 30. The downward trend that began in Q2 continued for all of the companies except Molina, which experienced a small net increase (+16,000). Centene reported the largest…
-
States Cannot Terminate CHIP Coverage for Non-Payment of Premiums Under 12-Months Continuous Eligibility Requirement
The Consolidated Appropriations Act, 2023 established a new requirement that all states provide 12-months continuous eligibility in Medicaid and the Children’s Health Insurance Program (CHIP) for children starting on January 1, 2024. Currently, only about half of the states have taken up the option to provide 12-months continuous eligibility for children in both programs. In…
-
Webinar: Medicaid Managed Care Organizations and Maternal Health
View Webinar Transcript Download the Presentation Slides