Blog
-
Children’s Marketplace Enrollment Increases Again, but Most Children Will Still be Eligible for Medicaid After Unwinding
When it comes to recent trends in children’s coverage, much attention has rightly focused on the significant child enrollment increases in Medicaid over the past few years due in large part to the Medicaid continuous coverage requirement. Although the Marketplaces cover far fewer children by comparison, child enrollment in Marketplace plans has increased substantially for…
-
Data Dashboards Offer Transparency to Medicaid Unwinding Process
As Unwinding Wednesday blog readers know, we are obsessed with data. We’ve highlighted key data to use to monitor the unwinding (performance indicators and supplemental unwinding data), stressed the importance of monitoring call center statistics as they will be the canary in the coalmine, and dug into the nuances of data on procedural disenrollments. And…
-
A World Without The ACA’s Preventive Services Protections: The Impact Of The Braidwood Decision
[Editor’s Note: On April 13, the U.S. Department of Justice requested a stay while it pursues an appeal of the Braidwood decision.) By Sabrina Corlette On March 30, 2023, a federal district court judge issued a sweeping ruling, enjoining the government from enforcing Affordable Care Act (ACA) requirements that health plans cover and waive cost-sharing for…
-
Black Mamas Matter Alliance Highlights Policy Change Needed in Honor of Black Maternal Health Week
Today marks the end of Black Maternal Health Week, which is celebrated every year from April 11-17. This initiative was founded by the Black Mamas Matter Alliance (BMMA), which advocates for Black mothers and has goals of changing policy, cultivating research, advancing care, and shifting culture. The week calls attention to the Black maternal health…
-
Speaker McCarthy Blames Medicaid for the Labor Shortage! Huh??
“Right now there are more job openings than people who are looking for jobs. You know why? It’s in part because the Biden Administration weakened work requirements. Incentives matter.” While that quote sounds like a line from a Saturday Night Live skit, it’s actually from Speaker McCarthy’s speech today on Wall Street outlining the House…
-
DACA Grantees Move Step Closer to Affordable Health Coverage
The Biden Administration made an important announcement today – the Department of Health and Human Services (HHS) will soon release a proposed rule that would finally give Deferred Action for Childhood Arrivals (DACA) grantees access to health care coverage. Under current law, DACA grantees are ineligible for Medicaid, CHIP, and Marketplace coverage even though other,…
-
Birthing With Dignity and Facing the Disparities: My Black Maternal Health Week Reflections
By Marquita Little Numan As we recognize Black Maternal Health Week this year, I wanted to take a moment to reflect on my personal birth experience as a Black mother. In 2021, as we all adjusted to a new normal and navigated life during a pandemic, my family was thankful for a reason to celebrate. We learned…
-
What Do the Data Tell Us about the Unwinding of the Medicaid Continuous Enrollment Requirement?
When watching a baseball game, we rely on the scoreboard to keep track of the score, strikes, balls, outs, etc. But unfortunately, it’s not quite that simple when it comes to keeping up with the Medicaid continuous coverage winddown. So far, we have very little data available to monitor the unwinding. CCF is posting state…
-
What Happens when the Medicaid “Unwinding” Meets a Natural Disaster?
It turns out that you can’t schedule natural disasters. They happen and they don’t particularly care when. Most recent case in point: Two weeks ago, tornados devastated three counties in Arkansas and six counties in Mississippi, resulting in approval of federal disaster assistance by President Biden and, in the case of Mississippi, a Public Health…
-
First Round of Medicaid Disenrollment Data Is In Quickly: What We Know and Don’t Know
Five states (AR, AZ, ID, NH, SD) started disenrolling people from Medicaid last weekend (April 1st) as the unprecedented Medicaid “unwinding” begins. As readers of SayAhh! know, in exchange for extra federal funds, states have been prohibited from disenrolling anyone involuntarily from Medicaid since March 2020 due to the COVID-19 public health emergency. Quicker than…
-
Unwinding Wednesday #27: States Should Figure Out a Way to Share Renewal Month with Enrollees, Assisters, and Health Care Providers
In mid-2022, only a little more than a third of enrollees had awareness of the unwinding of the Medicaid continuous enrollment requirement based on analysis conducted by the Urban Institute. As awareness of the resumption of Medicaid renewals and disenrollments is increasing, some enrollees are getting anxious. And the best way to help quell their…
-
New Brief: An Introduction to Managed Care in CHIP
Some three million kids in states with separate CHIP programs are enrolled in Managed Care Organizations (MCOs). Who are those MCOs, and how are they performing for those children? Unlike Medicaid, there’s no publicly available national database that answers those questions. Our new brief attempts to fill that gap. We utilized a variety of methods,…
-
We Just Checked and Medicaid Work Requirements are Still a Terrible Idea
Our world is constantly in flux and that can be stressful. But you can rest assured that Medicaid work requirements are a consistently and unalterably terrible idea. The years may pass, but some things never change. Just a few short years ago, numerous experts weighed in on the expected harms associated with Medicaid work requirements.…
-
Unwinding Wednesday #26: As the Medicaid Continuous Coverage Protection Ends This Week, It’s Important to Understand Procedural Disenrollments and Why They Occur
Friday, March 31, 2023, will be the last day that Medicaid enrollees are protected from a loss of Medicaid coverage. As of April 1st, people will begin to lose their coverage if they are determined ineligible and many of those will encounter barriers in transitioning to other coverage. These include affordability, limited special enrollment periods…
-
Research Update: Are We Underestimating the Number of Children?
Two recent data analyses highlight a question researchers have been asking for years: why is it so hard to get an accurate count of the number of children and is the undercount getting larger? First, a new report from Count All Kids looks at how well—or rather, poorly—children were counted in the 2020 decennial Census,…
-
Medicaid Coverage At Risk for People with Disabilities: How You Can Help
By Michael Atkins, The Arc of the United States Medicaid is the nation’s primary health insurance for people with disabilities, covering over ten million people with disabilities under the age of 65. For many people with intellectual and developmental disabilities (IDD), Medicaid provides even more than insurance – it’s a lifeline. Millions of people with…
-
Join Us in Welcoming Hannah and Tanesha to CCF Team
Georgetown University Center for Children and Families is happy to welcome two new members to our team: Hannah Green and Tanesha Mondestin. Hannah Green joins us as the new communications manager. In this role, she will work with CCF Communications Director Cathy Hope to share CCF’s research and analysis with you and others through our…
-
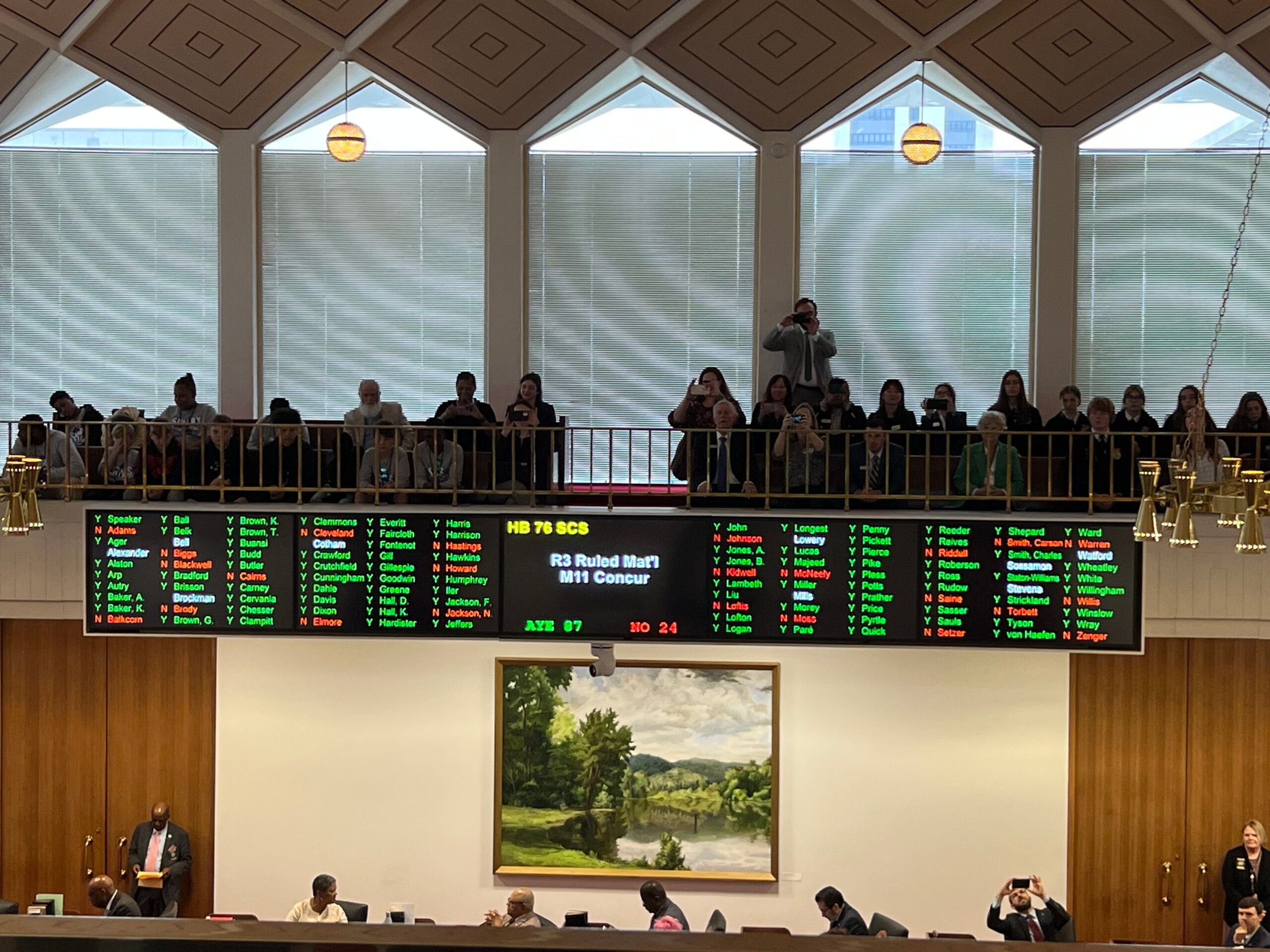
North Carolina’s Legislature Passes Medicaid Expansion
Today North Carolina’s Legislature passed Medicaid expansion in a bipartisan vote of 87-24. North Carolina’s Governor is expected to sign the bill early next week. This is a huge victory for better health care that will affect over 600,000 North Carolinians. I wrote last week about the multiple factors that set the stage for expansion…
-
Celebrating Health Care Gains Ushered in by Affordable Care Act
It’s been 13 years since the Affordable Care Act (ACA) was signed into law. At the time my daughter was in elementary school and I didn’t much think about what would happen to her health insurance – but now as she seems very grown up and is about to graduate from college and search for…
-
Child Medicaid/CHIP Coverage by School District Now Available
[Editor’s Note: These maps were updated on August 3, 2023. See here for updated data.] As we’ve written before, Medicaid is an essential tools for supporting schools in improving children’s health, especially mental health. Research has shown that Medicaid coverage can help boost children’s school readiness and reduce absenteeism, as well as improve high school…