Blog
-
Lessons from the Pandemic: Children’s Coverage Improvements
As readers of SayAhhh! know, Medicaid and CHIP enrollment is at an all-time high with close to 86 million people – covering half of the country’s children. Children and adults on Medicaid are protected by the continuous coverage provision including in the Families First Act (link to explainer) that prevents states from disenrolling anyone involuntarily.…
-
Once Again, Secretary Becerra Extends the PHE: What Does This Mean for the Medicaid Continuous Coverage Protection?
[Editor’s Note: Read the latest on the public health emergency Medicaid continuous coverage protection here.] It’s no surprise that HHS Secretary Becerra has renewed the COVID-related public health emergency (PHE) until July 15, 2022, since the Biden administration did not signal an end to the PHE 60 days in advance of the April 16, 2022…
-
New Florida Law Requires Stratified Performance Measure Data for Medicaid Managed Care
By Anne Swerlick, Senior Policy Analyst, Florida Policy Institute Experts agree that to reduce health disparities, you first need to know where they exist. The collection of health plan performance measure data, such as timely prenatal care and well-child check-ups, broken down by demographic factors like race and ethnicity is essential for developing targeted health…
-
Medicaid Managed Care Compliance Tools: Another ‘Pay-For’
Discussions have begun on the possibility of enacting a scaled-down version of the Build Back Better legislation. Any agreement that includes new federal spending will also require pay-fors (a/k/a offsets) either in the form of spending reductions or tax increases, or both. In Medicaid, responsible pay-fors—i.e., policy changes that the Congressional Budget Office will score…
-
At Long Last, the Biden Administration Takes Step to Fix the Family Glitch
Back in 2014, I wrote about the importance of fixing the family glitch in this Health Affairs policy brief, which I, along with other health policy wonks, thought could be fixed administratively through rule-making. At last, the Biden administration has announced steps to do so with a White House event featuring former President Obama, whose…
-
North Carolina: A Bipartisan Effort to Expand Medicaid Coverage and Improve Access to Healthcare
Last month, my colleague Adam Searing wrote a blog post about the status of Medicaid expansion in five states (South Dakota, North Carolina, Wyoming, Missouri, and Mississippi) twelve years after the passage of the Affordable Care Act. This week, we’re taking a closer look at one of these states, North Carolina, which is on a…
-
One Year of Medicaid Postpartum Coverage Option Begins Today, More Approvals to Come
Today marks the start of a significant policy change that will extend lifesaving health coverage to hundreds of thousands of pregnant and postpartum people each year: the American Rescue Plan’s option to extend postpartum coverage from 60 days to one year after the end of pregnancy. CMS announced today that Louisiana was the first state…
-
Research Update: Who Experiences Medical Debt?
Nearly 1 in 10 adults held significant medical debt in 2019, according to a new analysis from The Peterson Center on Healthcare and the Kaiser Family Foundation (KFF). Using data from the Census Bureau’s Survey of Income and Program Participation (SIPP), researchers found that about 23 million people owed at least $250 in unpaid medical…
-
Medicaid Pregnancy Coverage Fills a Critical Health Insurance Gap During Pandemic, Data Shows
Among all the Medicaid beneficiaries who’ve had their health coverage protected through the COVID-19 public health emergency, pregnant women stand out, new data released from CMS show. As readers of the SayAhhh! Blog know, the Families First Coronavirus Response Act included a “continuous coverage” provision that linked receipt of enhanced federal Medicaid and CHIP funding…
-
CMS Issues New Guidance on Variable Best Price Reporting under the Medicaid Drug Rebate Program
On March 23, 2022, the Centers for Medicare and Medicaid Services (CMS) released new technical guidance to drug manufacturers and states related to the highly effective Medicaid Drug Rebate Program (MDRP). The guidance is related to a rule finalized late in the Trump Administration that, among other provisions, allowed manufacturers to report a range of…
-
Research Update: Children’s Anxiety and Depression on the Rise
In a new article published last week in JAMA Pediatrics, researchers from the Health Resources and Services Administration find that anxiety and depression among children ages 3-17 have increased over the last five years. The researchers use data from the National Survey of Children’s Health to look at trends in children’s health, care utilization, and…
-
CMS Shares State Reporting Requirements on PHE Unwinding, but Will the Agency Share State Reports with the Public?
We’ve been expecting CMS to release a template for states to report key baseline and monthly data that is needed to monitor the unwinding of the Medicaid continuous coverage protection, but we got more than that with today’s release. CMS will also require states to complete and submit a form that summarizes the state’s approach…
-
Medicaid Expansion Discussion in Selected States Twelve Years After ACA Passage
This week marks the twelve-year anniversary of the Affordable Care Act (ACA) but residents of twelve states still have not been able to access the Medicaid expansion benefit enacted as part of that law as their state leaders have blocked it from taking effect. Over two million Americans are still unable to get quality, affordable…
-
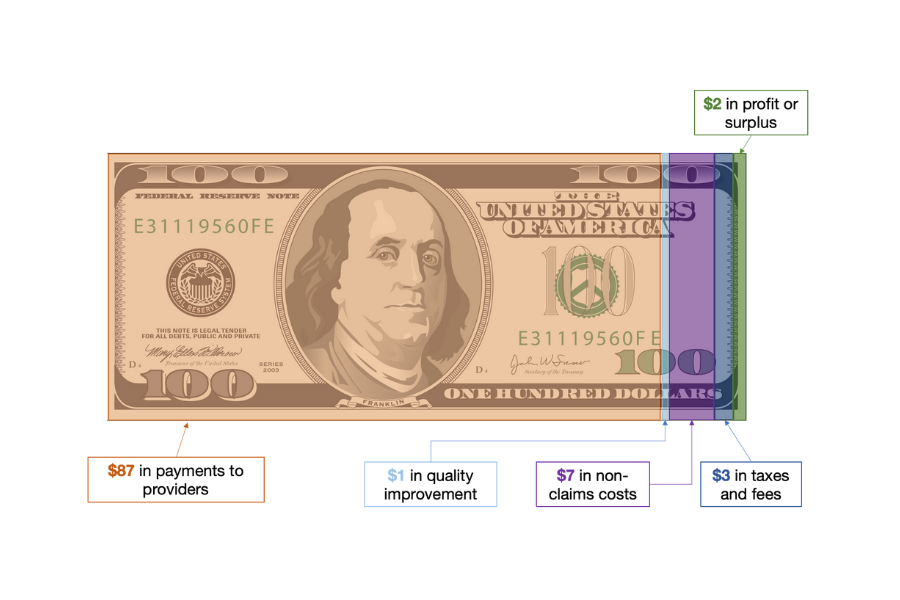
Medicaid Managed Care: SDOH, MCO, and MLR
There is no shortage of acronyms or initialisms in government agencies and programs and Medicaid is no exception. The Medicaid and CHIP Payment and Access Commission or MACPAC (one of our favorite acronyms) devotes an entire glossary to them. The most prominent initialism in Medicaid policy discussions these days is SDOH: social determinants of health,…
-
More States Make Progress on Extending Postpartum Medicaid Coverage
The 2022 state legislative season is nearing its end in the coming weeks, and this year we’ve continued to see significant efforts in a broad range of states working to extend the Medicaid postpartum coverage from the current cutoff of just 60 days to a full 12 months after the end of the pregnancy. Regular…
-
CMS Releases New Guidance on Unwinding the Medicaid Continuous Coverage Requirement
Yesterday, CMS released additional guidance and tools for states and Medicaid stakeholders on resuming routine operations when the Medicaid continuous coverage provision is lifted at the end of the public health emergency (PHE). While the State Health Official (SHO) reinforces prior guidance, it also provides new content and emphasizes the importance of protecting enrollees from…
-
Medicaid Managed Care: What Can the Annual MLR Report Tell Us?
Over 32.8 million children are covered by Medicaid, and the large majority are enrolled by their state Medicaid agencies in managed care organizations (MCOs). In exchange for monthly capitation payments, the MCOs contract with the state Medicaid agency to furnish covered services through networks of providers. These arrangements, in 40 states and the District of…
-
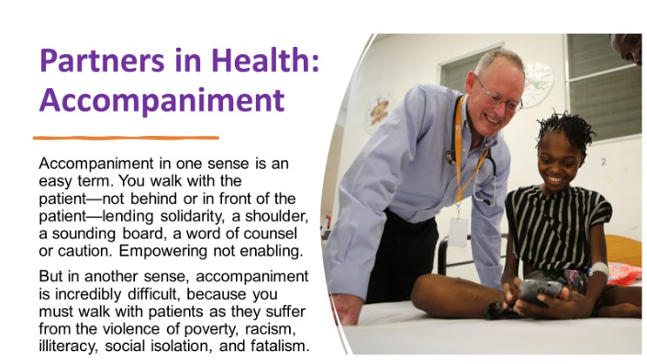
Reflecting on the Legacy of Dr. Paul Farmer
By Charles Bruner, Ph.D., Director of the Integrated Care for Kids The health community is saddened by Dr. Paul Farmer’s death – but also heartened by the many tributes to his life and the path he has presented for us. Although much of his work focused upon the poorest and most distressed communities in the…
-
Increase in Maternal Mortality During COVID Underscores Need for Policy Changes
The rate of women who died during pregnancy or shortly after birth increased significantly during the first year of the COVID-19 pandemic, according to new data from the National Center for Health Statistics, and Black women continued to experience maternal death at rates more than twice the national average. In 2020, there were 861 women…
-
Congressional Committees Focus on Mental Health, Announce Bipartisan Efforts
Mental health was in the spotlight this month on Capitol Hill with four Congressional committees holding hearings on the subject during the first three weeks of February and some committees formally announcing plans to pursue bipartisan legislation. As we’ve discussed on Say Ahhh!, the pandemic has taken an unprecedented toll on the mental health of…