Research & Reports
-
Georgia’s Women of Reproductive Age Face Many Barriers to Health Care
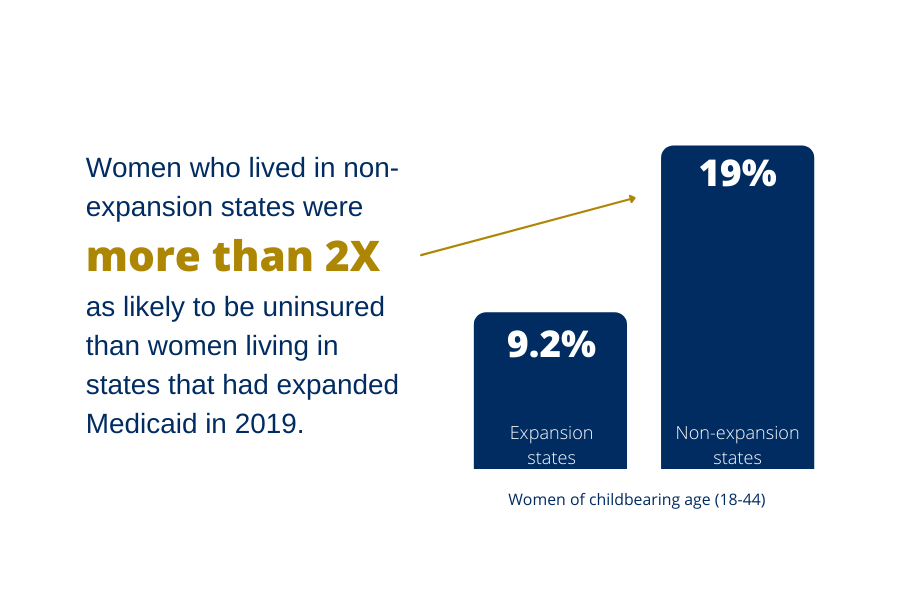
One in Five Women of Reproductive Age Is Uninsured in Georgia Largely due to the state’s decision not to expand Medicaid, Georgia has one of the highest rates of uninsured women of reproductive age (18-44) in the country with nearly one in five (19.3 percent) lacking health insurance. Georgia ranks 46th in the country and…
-
Opportunities to Support Maternal and Child Health Through Medicaid’s New Postpartum Coverage Extension
Introduction The new state option to extend Medicaid and CHIP coverage for one year after the end of pregnancy is a transformational opportunity for states to support improved maternal and infant health in the year following birth. It also offers state Medicaid leaders a focused moment to use the successful implementation of the new policy…
-
CHIP: Serving America’s Children for 25 Years
In its 25-year history, the Children’s Health Insurance Program (CHIP) has established itself as a critical piece of the federal-state response to children’s health care needs. CHIP, signed into law on August 5, 1997, was created to build on the success of Medicaid by giving states the opportunity to receive enhanced federal matching funds to…
-
A Guide for Health Care Advocates: Medicaid Managed Care Procurement
Overview Most Medicaid beneficiaries in most states are enrolled in managed care organizations (MCOs). (See text box, “What’s a Medicaid MCO?”) State Medicaid agencies contract with MCOs to assemble networks of health care providers to furnish services to program beneficiaries and protect them from medical debt. Simply put, if an MCO does not do its job,…
-
Response to Access RFI
Georgetown University Center for Children and Families submitted the following response to CMS’s request to identify strategies to ensure that individuals eligible for Medicaid and CHIP are able to apply, enroll in, and receive benefits in a timely and streamlined manner that promotes equitable coverage. CCF Response to Access RFI
-
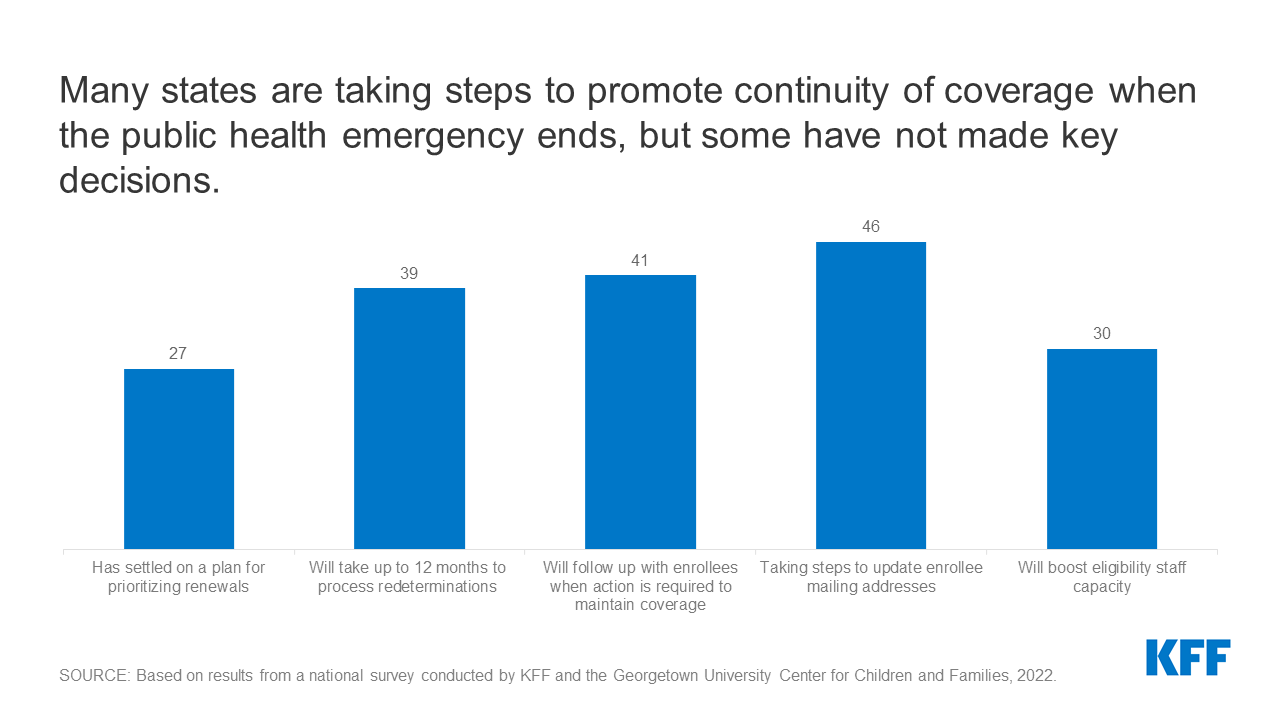
Medicaid and CHIP Eligibility and Enrollment Policies as of January 2022: Findings from a 50-State Survey
Executive Summary Enrollment in Medicaid has grown significantly during the coronavirus pandemic. Provisions in the Families First Coronavirus Response Act (FFCRA) require states to provide continuous coverage for Medicaid enrollees until the end of the month in which the public health emergency (PHE) ends in order to receive enhanced federal funding. Continuous enrollment has helped to preserve…
-
Millions of Children May Lose Medicaid: What Can Be Done to Help Prevent Them From Becoming Uninsured?
Introduction As of June 2021, over 40 million children were enrolled in Medicaid or CHIP for their health insurance — the vast majority in Medicaid. From the month prior to the pandemic in February 2020, through June 2021, children’s enrollment increased by 11 percent. Now, about half of the nation’s children are covered by Medicaid…
-
American Rescue Plan Home and Community-Based Services Funding: A Review of State Plans to Support Child and Adolescent Mental Health
The COVID-19 pandemic has taken an unprecedented toll on children’s mental health, exacerbating long-standing gaps in mental health care for children in the United States. Fortunately, a number of states plan to invest in initiatives that support youth behavioral and mental health by leveraging funds made available by section 9817 of the American Rescue Plan…
-
Gaps in Coverage: A Look at Child Health Insurance Trends
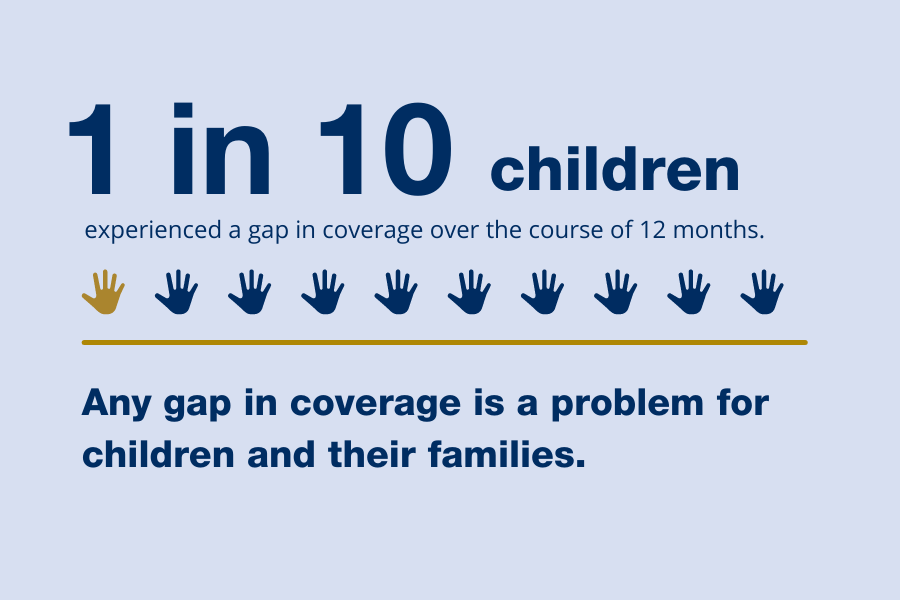
The number of uninsured children was on a downward trajectory for many years, but in 2017 started going back up, rising a full percentage point between 2016 and 2019 (see Figure 1). This issue brief examines the incidence and characteristics of children who experienced a period of uninsurance over the course of a recent year…
-
Build Back Better Act: Health Coverage Provisions Explained
On November 19, 2021, the House of Representatives passed the Build Back Better Act, the budget reconciliation bill, with the Senate expected to consider the legislation in coming weeks. The Build Back Better Act includes numerous provisions that would dramatically strengthen and expand both public and private health insurance coverage. Some of the new provisions…
-
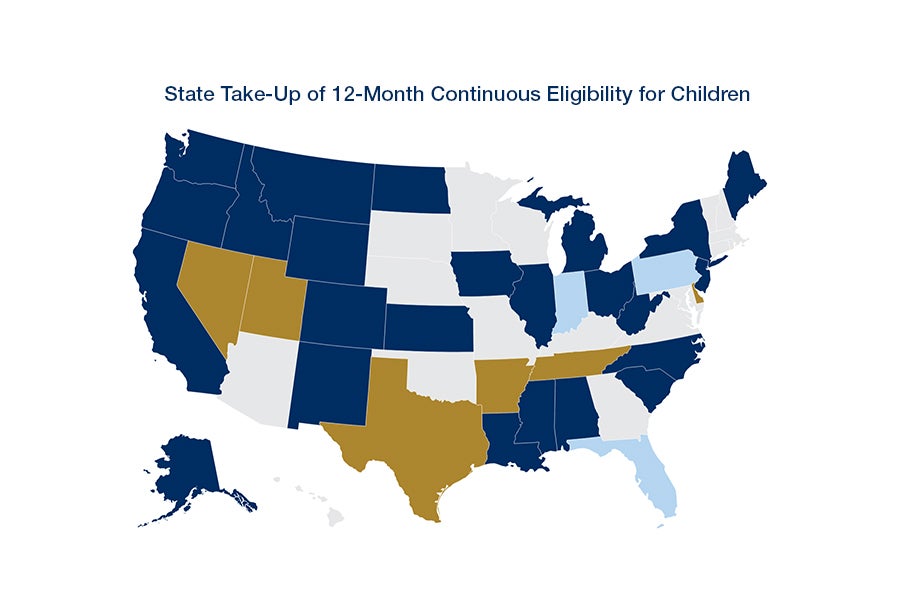
Advancing Health Equity for Children and Adults with a Critical Tool: Medicaid and Children’s Health Insurance Program Continuous Coverage
Key Takeaways: Latino children disproportionately receive their health coverage through Medicaid or CHIP. Together, these programs provide coverage for more than one-third (37.6 percent) of all children, but more than half (52.1 percent) of Latino children. Adopting Medicaid and CHIP policies that remove barriers to participation and reduce gaps in coverage would narrow inequities in…
-
Transparency in Medicaid Managed Care for Children and Youth in Foster Care
Executive Summary Children and youth in foster care are among the most vulnerable populations covered by Medicaid. When children and youth enter the child welfare system, they are often not up to date on routine care, and many have unrecognized and untreated medical needs. In addition, the experience of removal from a child’s biological family,…
-
Medicaid Expansion Narrows Maternal Health Coverage Gaps, But Racial Disparities Persist
Introduction The United States is experiencing a maternal mortality crisis and has the highest maternal mortality rate of any industrialized country in the world.8 In 2019, more than 750 women died of maternal causes in the United States while pregnant or within 42 days after the end of pregnancy, data from the Centers for Disease…
-
Transparency in Medicaid Managed Care: Findings from a 13- State Scan
Report Download the report. Appendix Online appendix tables. Blog Read the blog.
-
Future of Children’s Health Coverage: Next Steps for CHIP
The Children’s Health Insurance Program (CHIP) has established itself as a critical piece of the federal/state response to children’s health care needs. In addition to covering over 6 million children directly, CHIP has spurred outreach and enrollment simplification efforts that have resulted in more eligible children receiving Medicaid. Though children enrolled in separate CHIP programs…
-
Continuous Coverage in Medicaid and CHIP
Executive Summary Continuous health insurance coverage produces a broad array of benefits across the health care sector for individuals, states, health plans, and providers. In particular, Medicaid continuous eligibility promotes health equity by limiting gaps in coverage for low-income children and adults who experience disproportionate rates of health disparities. Consistent access to health care, including…
-
A Guide for Child Health Advocates: Medicaid Managed Care Accountability Through Transparency
Medicaid, Managed Care, and Transparency Medicaid is the nation’s largest health insurer for children—over 35 million at last count—and pays for nearly half of the nation’s births. It offers a comprehensive pediatric benefit—Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) services—for children and comprehensive maternity care for pregnant women. In most states, Medicaid agencies contract…
-
Urgent Action Needed to Catch Up on Routine Childhood Vaccinations
Introduction Vaccines are a safe and effective method of reducing the burden of infectious disease. On an individual level, they prevent severe illness, death, and long-term consequences of disease such as neurological disorders. On the community level, they forestall dangerous outbreaks of infectious disease and save money that would otherwise be spent on treating preventable…
-
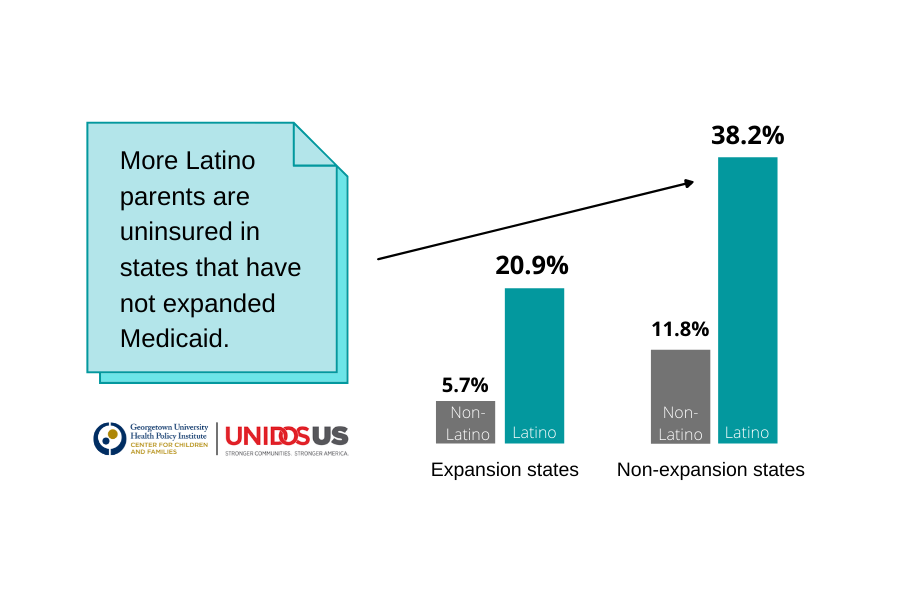
Expanding Medicaid Would Help Close Coverage Gap for Latino Children and Parents
Introduction The Affordable Care Act (ACA) has lowered the uninsured rate for children and families nationally, but its impact varies across the country based on whether a state has adopted the ACA’s Medicaid expansion to cover more adults.1 For Latino children and families, Medicaid serves an especially important role; while Latinos are more likely to…
-
A Profile of Florida’s Low-Wage Uninsured Workers
The recently enacted American Rescue Plan Act of 2021 (ARP) includes new large financial incentives for states to extend health insurance coverage to low-wage workers and other adults earning less than $17,775 a year.¹ These incentives apply to regular spending in a state’s Medicaid program and offer a five-percentage point across the board increase in the…