CHIP
-
State Medicaid and CHIP Options Can Help Address Maternal Health Crisis and Eliminate Racial Health Inequities
Two Say Ahh! blogs published during Black Maternal Health Week this April–one from Marquita Little Numan reflecting on her personal birth story and another by Tanesha Mondestin on the Black Mamas Matter Alliance policy agenda – underscored the need for significant policy change to address the ongoing maternal health crisis facing our country, where Black…
-
State Opportunities to Leverage Medicaid and CHIP Coverage to Improve Maternal Health and Eliminate Racial Inequities
Introduction Medicaid and CHIP provide coverage for millions of pregnant people to access essential prenatal, birth-related, and postpartum care each year.[1] Policymakers are taking a fresh look at Medicaid and CHIP options to support better maternal health outcomes in response to the nation’s worsening maternal mortality crisis, the 2022 Supreme Court decision in Dobbs v.…
-
Children’s Marketplace Enrollment Increases Again, but Most Children Will Still be Eligible for Medicaid After Unwinding
When it comes to recent trends in children’s coverage, much attention has rightly focused on the significant child enrollment increases in Medicaid over the past few years due in large part to the Medicaid continuous coverage requirement. Although the Marketplaces cover far fewer children by comparison, child enrollment in Marketplace plans has increased substantially for…
-
New Brief: An Introduction to Managed Care in CHIP
Some three million kids in states with separate CHIP programs are enrolled in Managed Care Organizations (MCOs). Who are those MCOs, and how are they performing for those children? Unlike Medicaid, there’s no publicly available national database that answers those questions. Our new brief attempts to fill that gap. We utilized a variety of methods,…
-
An Introduction to Managed Care in CHIP
DOWNLOAD THIS REPORT Introduction The Children’s Health Insurance Program (CHIP) was enacted 25 years ago. [1] Today it provides coverage for children whose family incomes are too high to allow them to qualify for Medicaid but too low to enable them to afford private health insurance coverage. Together, CHIP and Medicaid insure over half [2]…
-
Child Medicaid/CHIP Coverage by School District Now Available
[Editor’s Note: These maps were updated on August 3, 2023. See here for updated data.] As we’ve written before, Medicaid is an essential tools for supporting schools in improving children’s health, especially mental health. Research has shown that Medicaid coverage can help boost children’s school readiness and reduce absenteeism, as well as improve high school…
-
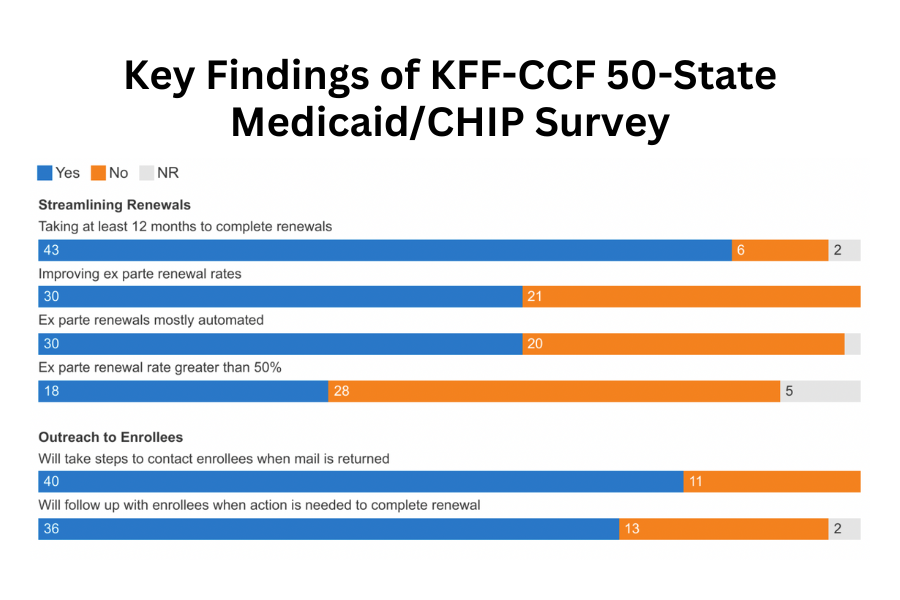
KFF-CCF Survey Provides Snapshot of Medicaid and CHIP at Watershed Moment as States Prepare for Unwinding Continuous Enrollment
The Kaiser Family Foundation (KFF) and Georgetown University Center for Children and Families annual 50-State Survey on Medicaid and CHIP Eligibility and Enrollment was released today. The survey focuses on state policies impacting children, pregnant individuals, parents, and other non-elderly adults whose Medicaid eligibility is based on financial eligibility rules. This year’s survey provides a…
-
Medicaid and CHIP Eligibility, Enrollment, and Renewal Policies as States Prepare for the Unwinding of the Pandemic-Era Continuous Enrollment Provision
Executive Summary In the third year of the COVID-19 public health emergency (PHE), Medicaid enrollment continued to increase albeit at a slower pace than in the first two years of the coronavirus pandemic. Since March 2020, states have provided continuous enrollment in Medicaid in exchange for enhanced federal funding. This continuous enrollment provision and enhanced…
-
Comments on Medicaid/CHIP Provisions in Proposed Rule on Prior Authorization
The Georgetown University Center for Children and Families submitted the following comments to CMS regarding the proposed regulation on prior authorization and interoperability. Prior Authorization Comments
-
Medicaid and CHIP Drug Rebate Proposals in the Biden Administration’s Fiscal Year 2024 Budget
Under the highly effective Medicaid Drug Rebate Program (MDRP), drug manufacturers must provide substantial rebates to the federal government and states as a condition of having their drugs covered by Medicaid. For brand-name drugs, the rebates apply to both fee-for-service and Medicaid managed care and consist of two mandatory components. First, under a basic rebate,…
-
Hundreds of Thousands of Children Could Lose Coverage in Florida Alone as U.S. Approaches High Stakes Medicaid Unwinding
As readers of SayAhhh! know, Congress has given the green light to states to begin checking eligibility for all Medicaid beneficiaries who have been protected from disenrollment by federal law since the Families First Covid Relief Act passed in March 2020. Terminations can begin on April 1, 2023; states have a year to complete the…
-
Unwinding Wednesday #15: Congress Proposes to End Medicaid Continuous Coverage Protection in Early 2023; Adds Transparency and Accountability Requirements
[Editor’s Note: The bipartisan spending plan was approved by Congress and signed into law by the President on December 29, 2022. Read CCF’s brief to learn more.] The text of the omnibus spending plan released by Congress would allow states to resume Medicaid disenrollments after the end of the first quarter…
-
Medicaid Unwinding Will Begin in April but There’s Good News in Congressional Funding Agreement
[Editor’s Note: The bipartisan spending plan was approved by Congress and signed into law by the President on December 29, 2022. Read CCF’s brief to learn more.] Congress has just reached an end of the year funding agreement, and it has very significant implications for the more than 90 million people who rely on Medicaid…
-
Congress Includes Medicaid, CHIP Mental Health Provisions in End of Year Funding Bill
[The bipartisan spending plan was approved by Congress and signed into law by the President on December 29, 2022. Read CCF’s brief to learn more.] As my colleagues on Say Ahhh! have highlighted the omnibus appropriations bill released earlier today includes a number of provisions related to Medicaid and CHIP such as funding for Puerto…
-
End of the Year Appropriations Bill Would Avert Medicaid Fiscal Cliff for Puerto Rico and the Territories
[Editor’s Note: The bipartisan spending plan was approved by Congress and signed into law by the President on December 29, 2022. Read CCF’s brief to learn more.] The bipartisan omnibus appropriations bill, which was unveiled early this morning by the Senate Appropriations Committee, would avert the dire Medicaid fiscal cliff facing Puerto Rico and the…
-
New Report Underscores Need to Reassure Immigrant Families
Researchers from the Urban Institute have documented the chilling effects of the Trump-era public charge regulation and other anti-immigrant policies for the past several years. Unfortunately, new research confirms that families are continuing to avoid public programs due to immigration-related concerns, despite having material hardships such as food insecurity, unmet medical needs, and problems paying…
-
Early Research Shows Benefits of One Year of Postpartum Medicaid
Over the last several months, we’ve seen the Biden Administration approve more than half of states to extend postpartum Medicaid coverage for one year after the end of pregnancy. Congress too has also considered proposals to require all states to offer 12 months of postpartum Medicaid coverage, which many advocates continue to champion to ensure…
-
Federal Focus on Behavioral Health Crisis Care
You may be thinking that we’ve been writing a lot about behavioral health on Say Ahhh! lately. Well, you’re right – and there’s more! For starters, last week, the Substance Abuse and Mental Health Services Administration (SAMHSA) released new National Guidelines for Child and Youth Behavioral Health Crisis Care, complementing other recent resources such as…
-
States Leading the Way on Connecting All Children with Health Coverage – Will Congress Follow?
According to the Urban Institute, over half of the remaining uninsured children are eligible for Medicaid or the Children’s Health Insurance Program (CHIP) but unenrolled. About a third of uninsured children are ineligible for Medicaid or CHIP because their family income exceeds the eligibility thresholds. Another 10% are ineligible for Medicaid/CHIP because of their immigration…
-
Comments on Streamlining Medicaid/CHIP Eligibility Determination, Enrollment and Renewal Processes
Georgetown University Center for Children and Families submitted these comments to CMS on the “Streamlining the Medicaid, Children’s Health Insurance Program, and Basic Health Program Application, Eligibility Determination, Enrollment, and Renewal Processes Proposed Rule.” EE NPRM CCF Comments