Medicaid
-
Unwinding Wednesday #27: States Should Figure Out a Way to Share Renewal Month with Enrollees, Assisters, and Health Care Providers
In mid-2022, only a little more than a third of enrollees had awareness of the unwinding of the Medicaid continuous enrollment requirement based on analysis conducted by the Urban Institute. As awareness of the resumption of Medicaid renewals and disenrollments is increasing, some enrollees are getting anxious. And the best way to help quell their…
-
Tips and Best Practices for Unwinding the Medicaid Continuous Coverage Protection
Unwinding the Medicaid continuous coverage protection will be a heavy lift. It will be important for states to work together with community partners in the planning process. Our new and improved Tips and Best Practices outline specific action steps states can take now to be better prepared for the end of the public health emergency…
-
We Just Checked and Medicaid Work Requirements are Still a Terrible Idea
Our world is constantly in flux and that can be stressful. But you can rest assured that Medicaid work requirements are a consistently and unalterably terrible idea. The years may pass, but some things never change. Just a few short years ago, numerous experts weighed in on the expected harms associated with Medicaid work requirements.…
-
Unwinding Wednesday #26: As the Medicaid Continuous Coverage Protection Ends This Week, It’s Important to Understand Procedural Disenrollments and Why They Occur
Friday, March 31, 2023, will be the last day that Medicaid enrollees are protected from a loss of Medicaid coverage. As of April 1st, people will begin to lose their coverage if they are determined ineligible and many of those will encounter barriers in transitioning to other coverage. These include affordability, limited special enrollment periods…
-
Medicaid Coverage At Risk for People with Disabilities: How You Can Help
By Michael Atkins, The Arc of the United States Medicaid is the nation’s primary health insurance for people with disabilities, covering over ten million people with disabilities under the age of 65. For many people with intellectual and developmental disabilities (IDD), Medicaid provides even more than insurance – it’s a lifeline. Millions of people with…
-
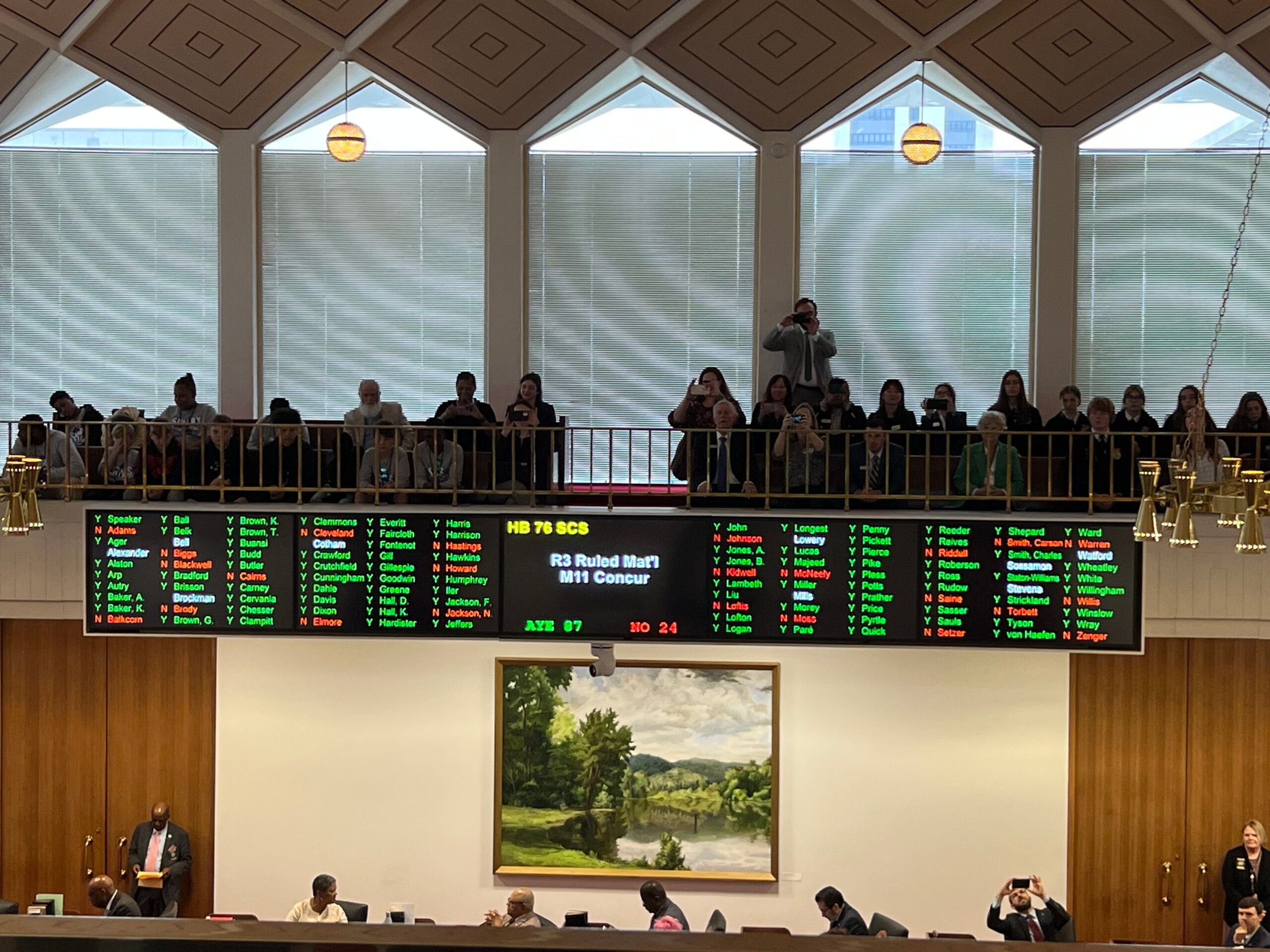
North Carolina’s Legislature Passes Medicaid Expansion
Today North Carolina’s Legislature passed Medicaid expansion in a bipartisan vote of 87-24. North Carolina’s Governor is expected to sign the bill early next week. This is a huge victory for better health care that will affect over 600,000 North Carolinians. I wrote last week about the multiple factors that set the stage for expansion…
-
Celebrating Health Care Gains Ushered in by Affordable Care Act
It’s been 13 years since the Affordable Care Act (ACA) was signed into law. At the time my daughter was in elementary school and I didn’t much think about what would happen to her health insurance – but now as she seems very grown up and is about to graduate from college and search for…
-
Child Medicaid/CHIP Coverage by School District Now Available
[Editor’s Note: These maps were updated on August 3, 2023. See here for updated data.] As we’ve written before, Medicaid is an essential tools for supporting schools in improving children’s health, especially mental health. Research has shown that Medicaid coverage can help boost children’s school readiness and reduce absenteeism, as well as improve high school…
-
Unwinding Wednesday #25: Renewal Reports Provide Important Insights to States’ Unwinding Plans
Next week, the continuous enrollment will expire and as a result, some families may lose coverage as soon as April 1. As states undergo final preparations for the unwinding to officially begin, state renewal reports are an important resource for stakeholders to prepare and help monitor the unwinding process. We covered the basics of the…
-
How Did We Get Here? An Early Legislative History of Medicaid Managed Care
Here is where we are today. Managed care—more precisely, comprehensive risk-based managed care—is the dominant delivery system in Medicaid. States can require beneficiaries to enroll in Medicaid managed care organizations (MCOs) in order to receive the health care services to which they are entitled, and 40 states now do so. MCOs can limit the network…
-
New Brief: States Focus on Improving Maternal Health Outcomes Amid Worsening Maternal Mortality Crisis
The U.S. continues to experience a worsening maternal mortality crisis that the COVID-19 pandemic only exacerbated. New data from the Centers for Disease Control and Prevention shows that the maternal mortality rate for all women nearly doubled between 2018 to 2021, climbing from 17.4 maternal deaths per 100,000 births in 2018 to 32.9 maternal deaths…
-
Medicaid Drug Rebate Program News and Notes
As part of its fiscal year 2024 budget, the Biden Administration proposed several Medicaid and CHIP policies related to the Medicaid Drug Rebate Program, which I covered in a recent blog. But over the last few months, there have been two other Medicaid drug rebate developments that are worth highlighting: Puerto Rico joins the Medicaid…
-
State Trends to Leverage Medicaid Extended Postpartum Coverage, Benefits and Payment Policies to Improve Maternal Health
Introduction Medicaid and the Children’s Health Insurance Program (CHIP) finance nearly half of all births each year, including a disproportionate share of births to women of color and women living in rural areas. *[1] Medicaid’s foundational role in maternity care financing presents a critical opportunity to leverage the program to respond to the ongoing U.S.…
-
HHS Awards Planning Grants to 15 States for Medicaid-Funded Behavioral Health Clinic Demonstration
This week, HHS announced that it awarded 15 states each with $1 million, one-year Certified Community Behavioral Health Clinic (CCBHC) planning grants in support of state efforts to join the Medicaid-funded CCBHC demonstration program. Awardees include: Alabama, Delaware, Georgia, Iowa, Kansas, Maine, Mississippi, Montana, North Carolina, New Hampshire, New Mexico, Ohio, Rhode Island, Vermont, and…
-
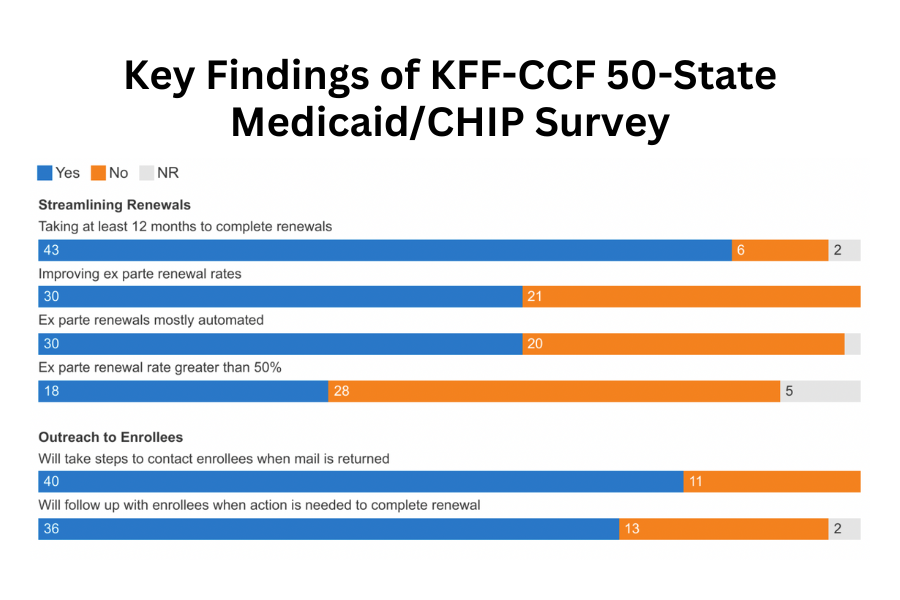
KFF-CCF Survey Provides Snapshot of Medicaid and CHIP at Watershed Moment as States Prepare for Unwinding Continuous Enrollment
The Kaiser Family Foundation (KFF) and Georgetown University Center for Children and Families annual 50-State Survey on Medicaid and CHIP Eligibility and Enrollment was released today. The survey focuses on state policies impacting children, pregnant individuals, parents, and other non-elderly adults whose Medicaid eligibility is based on financial eligibility rules. This year’s survey provides a…
-
Medicaid and CHIP Eligibility, Enrollment, and Renewal Policies as States Prepare for the Unwinding of the Pandemic-Era Continuous Enrollment Provision
Executive Summary In the third year of the COVID-19 public health emergency (PHE), Medicaid enrollment continued to increase albeit at a slower pace than in the first two years of the coronavirus pandemic. Since March 2020, states have provided continuous enrollment in Medicaid in exchange for enhanced federal funding. This continuous enrollment provision and enhanced…
-
Unwinding Wednesday #24: State-Specific Flyers Available Now to Inform Medicaid Enrollees About Upcoming Renewals
As my colleague Tricia Brooks wrote last week, the unwinding of the Medicaid continuous coverage provision is now underway in almost half of the states and in a handful of states, terminations for procedural reasons will begin next month. It is more important than ever to inform Medicaid enrollees about the changes that are coming…
-
Comments on Medicaid/CHIP Provisions in Proposed Rule on Prior Authorization
The Georgetown University Center for Children and Families submitted the following comments to CMS regarding the proposed regulation on prior authorization and interoperability. Prior Authorization Comments
-
Medicaid and CHIP Drug Rebate Proposals in the Biden Administration’s Fiscal Year 2024 Budget
Under the highly effective Medicaid Drug Rebate Program (MDRP), drug manufacturers must provide substantial rebates to the federal government and states as a condition of having their drugs covered by Medicaid. For brand-name drugs, the rebates apply to both fee-for-service and Medicaid managed care and consist of two mandatory components. First, under a basic rebate,…
-
If You Care About Children’s Mental Health, Here’s Why You Need to Care About Medicaid Unwinding
The pandemic has shed new light on children’s mental health across the nation. While the evidence is clear that even before the COVID pandemic there was a crisis in children’s mental health, the pandemic has further intensified the crisis, as highlighted by national pediatric provider groups in their declaration of a national emergency in child…