Eligibility & Enrollment
-
Expedited CMS Approvals in Washington and Oregon Can Further Minimize Coverage Disruptions, Aid Unwinding
New CMS approvals in Oregon and Washington will protect health coverage for more children and families during this year’s consequential unwinding, minimizing coverage disruptions and easing transitions to new sources of health coverage. Oregon receives approval to ease coverage transitions for certain adults, allowing them to stay in Medicaid until they can transition to alternative…
-
Children’s Marketplace Enrollment Increases Again, but Most Children Will Still be Eligible for Medicaid After Unwinding
When it comes to recent trends in children’s coverage, much attention has rightly focused on the significant child enrollment increases in Medicaid over the past few years due in large part to the Medicaid continuous coverage requirement. Although the Marketplaces cover far fewer children by comparison, child enrollment in Marketplace plans has increased substantially for…
-
Unwinding Wednesday #17: It’s Imperative for States to Use the 2023 Federal Poverty Levels During the Unwinding
The Assistant Secretary for Planning and Evaluation (ASPE) has released the 2023 federal poverty levels (FPL). As expected, there was a notable increase in the poverty threshold stemming from inflation that will help families keep pace with rising costs. On average, the FPLs rose by about 8 percent, ranging from 7.3…
-
Webinar: Medicaid Continuous Eligibility for Children up to age 6 in Oregon
On September 28, CMS approved Oregon’s groundbreaking proposal to provide continuous eligibility (CE) in Medicaid and CHIP for children from birth to age 6 as a component of the state’s school readiness and health care transformation strategies. The approval also creates a two-year CE for all beneficiaries ages 6 and older, along with a number…
-
Medicaid and CHIP Continuous Coverage for Children
States have the option under current law to provide 12 months of continuous health coverage for children in Medicaid and the Children’s Health Insurance Program (CHIP) so that children can maintain coverage throughout the year even as their family income fluctuates from month to month.[note]Twelve-month continuous eligibility was authorized in the 1997 Balanced Budget Act.…
-
What’s New for 2023 Marketplace Enrollment?
By Emma Walsh-Alker, Georgetown University Center on Health Insurance Reforms The annual open enrollment period for marketplace coverage is right around the corner. There are many new policies impacting the marketplace in 2023, including an extension of enhanced financial assistance through the Inflation Reduction Act; a federal fix to the “family glitch” that will create…
-
Child Uninsured Rate Declined During the Pandemic Thanks to Medicaid
New data from the American Community Survey (ACS) released today by the U.S. Census Bureau suggests that the continuous coverage provision of the Families First Coronavirus Response Act (which prohibits states from disenrolling anyone involuntarily from Medicaid during the duration of the federal COVID-19 public health emergency), has resulted in the child uninsured rate stabilizing and…
-
Proposed Eligibility Rule Simplifies Medicaid and CHIP Enrollment Process for Children
In a continuing effort to strengthen Medicaid and access to affordable, quality health coverage, the Biden Administration has proposed a series of eligibility rule changes. The Notice of Proposed Rulemaking (NPRM) seeks to streamline application and enrollment, improve retention rates, remove barriers specific to CHIP, and enhance program integrity. Eliminates enrollment barriers and benefit caps…
-
CHIP: Serving America’s Children for 25 Years
In its 25-year history, the Children’s Health Insurance Program (CHIP) has established itself as a critical piece of the federal-state response to children’s health care needs. CHIP, signed into law on August 5, 1997, was created to build on the success of Medicaid by giving states the opportunity to receive enhanced federal matching funds to…
-
New Urban Institute Analysis Underscores Importance of Continuous Medicaid Coverage Protection for Kids
A new brief out this week from The Urban Institute confirms what we have suspected — the Medicaid continuous coverage provision has halted the increase in uninsured children that we saw during the Trump years. (As SayAhhh! readers know, no one can be involuntarily disenrolled during the federally declared public health emergency as a consequence…
-
The Latest on Child Medicaid and CHIP Enrollment During the Pandemic
CCF’s Aubrianna Osorio and Allie Corcoran are keeping tabs on child enrollment in Medicaid and CHIP during the pandemic period. Below is the latest – from February 2020 to January 2022 child enrollment has increased by 14.4 percent nationwide. A few things jumped out at me: As is common, we are probably seeing “welcome mat”…
-
New CMS Resource is a Helpful Summary of Requirements for Unwinding the Continuous Coverage Protection
Over the past year and a half, CMS has released a variety of guidance, slide decks, tools, templates, and other resources on the unwinding of the continuous coverage provision. After a while, it can be pretty daunting to keep up with everything. Thankfully, the agency made it easier to find these resources by posting all…
-
More States Move to Expand Continuous Eligibility for Children and Adults in Medicaid
Waiver authorities granted through Section 1115 demonstrations are meant to be experiments that serve the objectives of the Medicaid program—namely, promoting access to health coverage. But what exactly does this look like? In some very welcome news, there has been a recent uptick in the number of states requesting to expand continuous eligibility through Section…
-
Child Uninsured Rate in 2021: Medicaid’s Continuous Coverage Provision is Helping
Children’s uninsured rate decreased from 2020 to 2021, according to new Early Release data from the Centers for Disease Control and Prevention’s National Health Interview Survey (NHIS). According to the NHIS, uninsurance for children under age 18 fell to 4.1 percent in 2021. Using this data source, the uninsured rate had remained steady at 5.1…
-
HHS and CMS Request FCC Opinion on Text Messaging by Contractors and MCOs
HHS Secretary Becerra and CMS Administrator Brooks-LaSure have formally asked for an opinion from the Federal Communications Commission (FCC) regarding whether certain text messages and automated, pre-recorded telephone calls to individuals’ cell phones are permissible under the Telephone Consumer Protection Act (TCPA). Prior rulings from the FCC have confirmed that neither federal nor state governments…
-
More Children Enrolled in ACA Marketplace Coverage in 2022, But Marketplaces Still Remain Modest Source of Health Coverage for Children
Medicaid and the Children’s Health Insurance Program (CHIP) currently cover more than 40 million children. In comparison, relatively few children rely on the marketplaces for their health coverage. But new data released by the Centers for Medicare & Medicaid Services (CMS) show 1.3 million children were enrolled in marketplace plans during the 2022 Marketplace Open…
-
Once Again, Secretary Becerra Extends the PHE: What Does This Mean for the Medicaid Continuous Coverage Protection?
[Editor’s Note: Read the latest on the public health emergency Medicaid continuous coverage protection here.] It’s no surprise that HHS Secretary Becerra has renewed the COVID-related public health emergency (PHE) until July 15, 2022, since the Biden administration did not signal an end to the PHE 60 days in advance of the April 16, 2022…
-
At Long Last, the Biden Administration Takes Step to Fix the Family Glitch
Back in 2014, I wrote about the importance of fixing the family glitch in this Health Affairs policy brief, which I, along with other health policy wonks, thought could be fixed administratively through rule-making. At last, the Biden administration has announced steps to do so with a White House event featuring former President Obama, whose…
-
CMS Shares State Reporting Requirements on PHE Unwinding, but Will the Agency Share State Reports with the Public?
We’ve been expecting CMS to release a template for states to report key baseline and monthly data that is needed to monitor the unwinding of the Medicaid continuous coverage protection, but we got more than that with today’s release. CMS will also require states to complete and submit a form that summarizes the state’s approach…
-
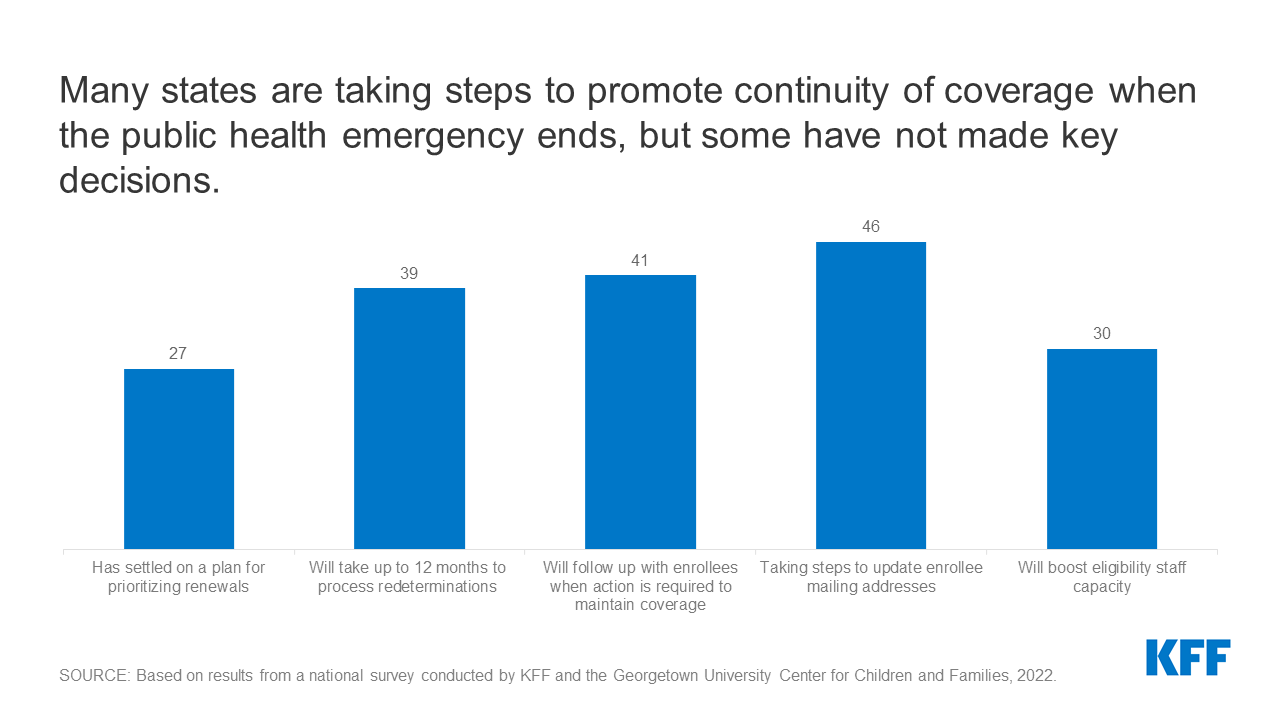
Medicaid and CHIP Eligibility and Enrollment Policies as of January 2022: Findings from a 50-State Survey
Executive Summary Enrollment in Medicaid has grown significantly during the coronavirus pandemic. Provisions in the Families First Coronavirus Response Act (FFCRA) require states to provide continuous coverage for Medicaid enrollees until the end of the month in which the public health emergency (PHE) ends in order to receive enhanced federal funding. Continuous enrollment has helped to preserve…