With the first week in May upon us, all 50 states have now begun initiating renewals for Medicaid enrollees, starting the clock on their unwinding process. We’ve already gotten a glimpse of what may be coming with data on coverage losses from Arizona and Idaho, both states that started terminations in April. The second wave of states started disenrolling people from Medicaid on May 1. There are many factors that may affect the scale of coverage losses from procedural disenrollments, but one of significant concern is notices.
States send notices to Medicaid and CHIP enrollees for a variety of reasons. For example, if an enrollee’s coverage is able to be renewed via ex parte, the state provides a notice to the enrollee that they remain eligible and coverage has been renewed. Or if an ex parte renewal is unsuccessful, the state sends an enrollee a notice that more information is needed to determine ongoing eligibility and that a renewal form must be completed. And if an individual is found no longer eligible for Medicaid or CHIP, they should receive a notice indicating the date their coverage will end as well as information about appealing the decision; this notice may also contain information about coverage options through the Marketplace. These are just to name a few.
With all these different types of notices, all of which require varying levels of action by enrollees, things can get confusing very quickly. While all notices are required to be written in plain language that can be easily understood, in reality many states have yet to do so. Especially if notices are sent out of order or it is not clear what steps enrollees need to take. This is why we emphasized the need for clear notices in plain language throughout our unwinding webinar series. It is essential that enrollees are able to clearly understand the notices they receive and actions required so they are able to maintain coverage or receive help to transition to other sources of coverage.
In an effort to get enrollees familiar with what they may receive in the mail, a handful of states have begun to post sample notices and/or renewal forms on their websites. These sample notices not only help members know what to look out for, but they also give stakeholders an opportunity to see where potential confusion in the notices exist or where states have taken steps to make notices clearer. Vermont’s sample renewal notice is a good example of this – it details all the ways individuals can submit their renewal form (including the steps for completing a paper renewal via mail) and the enrollee’s response deadline right at the top. The first page of the notice also includes information for interpretation services for enrollees with limited English proficiency.
In addition to using plain language, termination notices must state clearly and concisely what action the state is taking along with the reasons for taking those actions, and explaining the right to appeal a decision. The National Health Law Program (NHeLP) recently published a checklist with red flags to look for that may indicate non-compliance with notice or other redetermination requirements. Virginia has posted a sample termination notice, which is a great model as it clearly states the reason for termination, provides specific information on how to appeal the agency’s decision if the enrollee thinks a mistake has been made, and contains details on account transfers to the Marketplace and how to get assistance enrolling in that coverage.
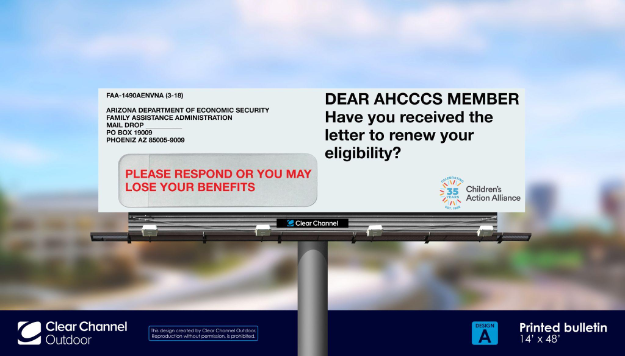
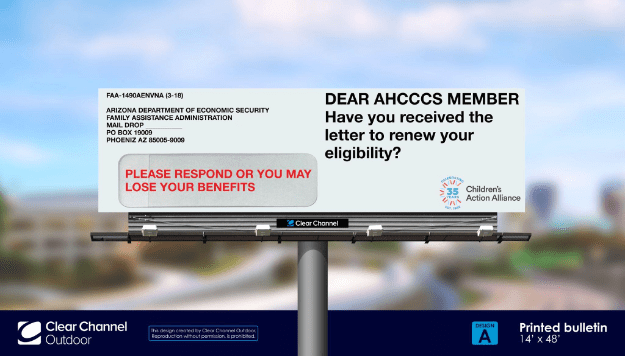
A final piece in the notices’ puzzle is ensuring that individuals actually receive Medicaid notices, most importantly renewal forms and/or those that indicate needed actions to maintain coverage. All states have been undertaking “update contact information” campaigns to make sure notices get to enrollees in the first place. But a number of other states are taking additional steps to help ensure important notices aren’t accidentally overlooked. Texas plans to send out renewal notices in bright yellow envelopes with “ACTION REQUIRED” in red lettering while Hawaii has opted to use both pink envelopes and pink letters for its renewal notices. These strategies will likely be especially effective when coupled with complementary communications about renewal notices, like Arizona’s new billboard campaign (shown below) that shows members what their renewal envelopes will look like.
Notices will be a critical part of states’ successes or struggles in their unwinding processes. Some members have not renewed their coverage in over three years, while others who enrolled during the continuous enrollment protection might be renewing their Medicaid for the very first time. Clear language, instructions, and information on where to get assistance can make a difference between a member retaining or losing their healthcare coverage.
[Editor’s Note: This is the 31st blog in the Unwinding Wednesday series. For more information, visit our PHE Unwinding resource page where you’ll find other blogs in this series, reports, webinars and the 50-state tracker.]