2023
-
Medicaid Managed Care: Transparency of Performance on Maternal Health
Our nation is in the midst of an ongoing maternal health crisis, one that particularly affects Black women. The causes are complex, the need to address them is urgent, and there is no single solution. One of many potential solutions that has not received enough attention is Medicaid managed care. Medicaid, the nation’s largest health…
-
Marketplace Enrollment During Medicaid Unwinding Ticked Up in June but Remained Modest
I have been regularly reporting on monthly data (here and here) from the Centers for Medicare and Medicaid Services (CMS) on the number of people who were either previously enrolled in Medicaid or had experienced a denial or termination who then selected a marketplace plan. At the end of September, CMS issued new data for…
-
Medicaid Managed Care, Maternal Mortality Review Committees, and Maternal Health: A 12-State Scan
Download the Full Report Introduction The United States is in the midst of an ongoing maternal mortality crisis and Medicaid, the health insurer for low-income Americans, has an important role to play in addressing it. Medicaid is the nation’s single largest maternity care insurer, paying for more than 40% of all births on average across all states,…
-
CMS Makes the Right Call on Utah’s Medicaid Waiver: Where Do Things Stand on Postpartum Coverage?
In a little-noticed but important action, CMS recently notified the Utah Medicaid agency that it should proceed with extending postpartum coverage from 60 days to 12 months under the state plan amendment (SPA) option rather than continuing to pursue its Section 1115 waiver request. At first blush, this seems like a distinction only the most…
-
How Did We Get Here? A Recent Legislative History of Medicaid Managed Care
Just over 25 years ago, Congress enacted a major change in federal policy on Medicaid managed care. It eliminated the 75/25 rule—the requirement that no more than 75 percent of the enrollees in a Medicaid managed care organization (MCO) could be Medicaid or Medicare beneficiaries. The logic of the rule was that if an MCO…
-
Black Maternal & Mental Health Summit Highlights the Urgency for Policy and Practice Change
In July, I had the chance to attend the Black Maternal & Mental Health Summit hosted by the Shades of Blue Project. Founder Kay Matthews established Shades of Blue in 2013 after the loss of her stillborn daughter. With worsening maternal morbidity rates in the United States, Kay has turned to advocacy as a way…
-
Unwinding Data Recap: What Do We Know So Far?
Last Friday marked the end of the month, which meant the release of new unwinding data from CMS. This time, though, CMS not only published data on renewal outcomes for June, but also posted preliminary outcome data for July, cutting the time lag to two months. As a result, there is now unwinding data available…
-
CMS Releases Guidance on 12-Month Continuous Eligibility for Children
CMS has released long awaited guidance to states on implementing 12-month continuous eligibility (CE) for all children in Medicaid and the Children’s Insurance Program (CHIP) under the age of 19 as enacted by Congress in the Consolidated Appropriations Act. As of January 2023, 26 states cover some or all children in Medicaid for a full…
-
HHS Takes Action on Maternal Mental Health Initiatives, Requests Input on Medicaid/CHIP Parity Compliance
Last week, the Administration announced a number of actions related to mental health with a focus on maternal health as well as parity in Medicaid and the Children’s Health Insurance Program (CHIP). Here’s a readout of the latest actions: Maternal Health Funding: HHS announced awards of more than $103 million to support and expand access…
-
AAP and CCF Release 2023 State Snapshots on the Importance of Medicaid for Children’s Coverage
Starting back in 2017 we created state snapshots with our colleagues at the American Academy of Pediatrics that show who Medicaid covers in each state, with a particular emphasis on Medicaid’s role in covering children. After a hiatus during the pandemic, we’ve updated the easy-to-understand 2-pagers with all the latest data on how Medicaid helps…
-
State Medicaid and CHIP Snapshots, 2023
The Georgetown University Center for Children and Families (CCF) and the American Academy of Pediatrics (AAP) created factsheets underscoring the importance of Medicaid in providing coverage for children in all 50 states and the District of Columbia. Sources available here. Previous snapshots can be found here (2019), here (2018) and here (2017). Check out more interactive…
-
New Resource Helps Pediatricians Inform Families on How to Keep Eligible Children Enrolled in Medicaid
We recently learned that one of the most effective tools for keeping eligible people enrolled in Medicaid – automated or “ex parte” renewals – has not been set up correctly in 30 states, including DC, while other states, such as Texas, are barely using automated systems at all. As Say Ahhh! readers know, Medicaid eligibility…
-
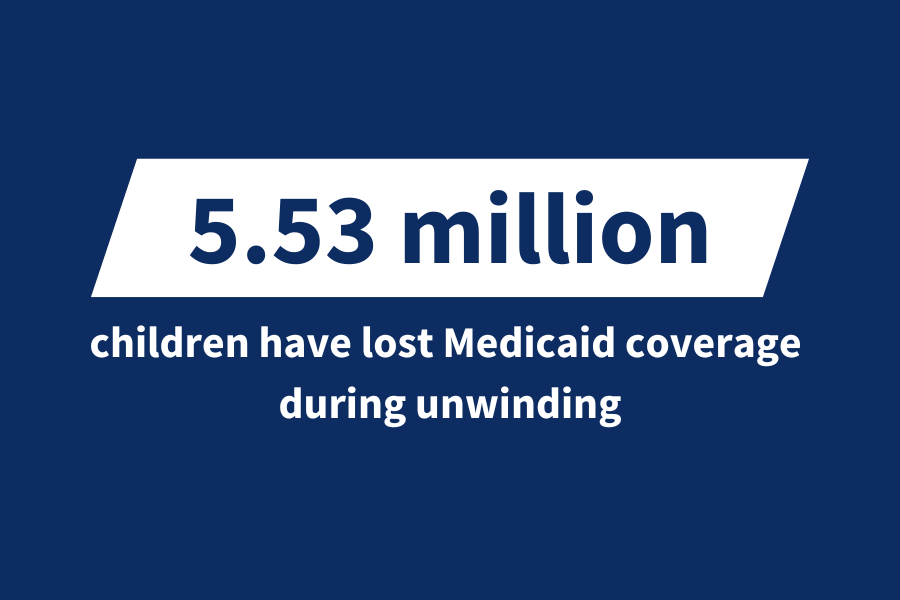
How many children are losing Medicaid?
The analysis on this page is part of a larger suite of Medicaid unwinding data. Please visit our “Unwinding the PHE” landing page to view more. As of March 2023, more than 35.1 million children were enrolled in Medicaid and approximately 4.3 million were enrolled in Medicaid coverage funded by CHIP—more than half of all U.S.…
-
Medicaid Support for Infant and Early Childhood Mental Health: Lessons from Five States
By: Kay Johnson and Elisabeth Burak Five states’ journeys to strengthen Medicaid support for infant and early childhood mental health (IECMH) –California, Colorado, Michigan, North Carolina, and Washington — offer lessons for other states seeking to more effectively prevent, identify, and address mental health conditions among young children in Medicaid. Lessons speak to the importance of: 1. Leadership…
-
Looming Government Shutdown Could Undermine Federal Oversight of Medicaid Unwinding
[Editor’s Note: On September 30, Congress approved a last-minute measure to fund the government through November 17, 2023, which temporarily averted a government shutdown. CCF experts will continue to monitor the funding debate and its impact on health care programs and the people who rely on them.] Sadly, we’ve been here before and it’s highly…
-
CBO Confirms House Bill Prohibiting Use of “QALYs” Would Undermine State Negotiation of Medicaid Supplemental Rebates
I previously raised significant concerns about a House health bill that would expand an existing Medicare prohibition on the use of Quality-Adjusted Life Years (QALYs) to other federal programs including Medicaid and the Children’s Health Insurance Program (CHIP). I warned that the bill was overbroad in its prohibition of the use of QALYs and could…
-
CMS Takes Swift Action to Require States to Address Medicaid Auto-Renewal Errors and Reinstate Children’s Coverage
We have long feared that large numbers of children were losing Medicaid during the unwinding, essentially by mistake, and the ex parte debacle underscores the fact that this is indeed happening. As we’ve previously explained, the ex parte issue came to light in August after a CMS investigation found several states were doing automatic renewals…
-
Midwives Offer State Medicaid Agencies Another Tool to Address the Maternal Health Crisis
Doulas have been a popular topic in the maternal health space as one means of improving birthing outcomes, especially for Black women and other communities of color that have been historically marginalized from the traditional health system. It can be confusing to differentiate between the different support persons and clinicians that may assist expecting or…
-
House Republican Budget Resolution Includes Draconian Medicaid Cuts
Yesterday, on September 19, 2023, House Budget Committee Chair Jodey Arrington issued a House budget resolution for fiscal year 2024 that would cut federal Medicaid spending by $1.9 trillion — or nearly 28 percent — over the next 10 years. While the budget resolution includes very little detail, it offers some indication about how the…
-
Update on Medicaid Unwinding and Marketplace Enrollment
I previously reported that according to data from the Centers for Medicare and Medicaid Services (CMS), of the 715,000 Medicaid beneficiaries who lost Medicaid coverage in April due to unwinding of the Medicaid continuous coverage protection, a total of about 54,000 people or 7.5 percent — who were either previously enrolled in Medicaid in March…