Eligibility & Enrollment
-
What Can States Do to Reduce Risk of Children Unfairly Losing Health Insurance
In part 1 of this blog series, my colleague and report co-author Joan Alker, explained the dire consequences if states don’t put in the time and effort to get renewals right when the Medicaid continuous coverage provision is lifted. This blog will focus on how we developed risk assessments for children in all 50 states…
-
Research Update: More than 1 in 3 Children Lacked Access to Adequate Coverage in 2019
Regular readers know that, since record lows in 2016, child uninsurance has been climbing in recent years. Regular readers also know that uninsured rates don’t give a full picture of children’s coverage. Similar to our recent paper on kids who experience coverage gaps, a new article in Pediatrics shows that just having some health insurance…
-
A Few Key Data Points Are Essential in Monitoring Medicaid Enrollment When the Continuous Enrollment Requirement is Lifted
The lifting of the continuous enrollment requirement associated with the COVID-19 public health emergency (PHE) is inevitable, whether it be after the PHE ends or on April 1, 2022 as proposed in the Build Back Better (BBB) Act passed by the House. Regardless of what happens, millions of enrollees are likely to be disenrolled from…
-
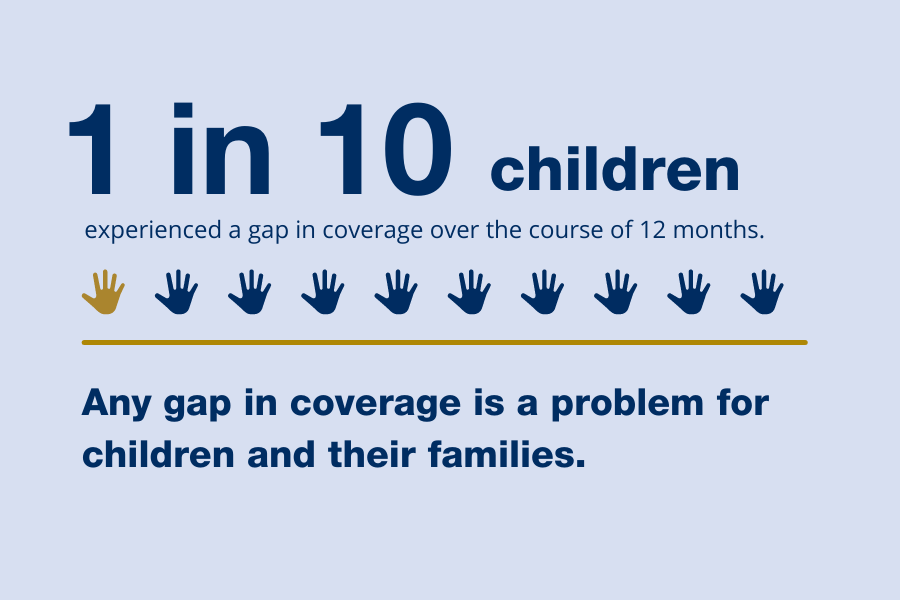
Gaps in Coverage: A Look at Child Health Insurance Trends
The number of uninsured children was on a downward trajectory for many years,[note]The Future of CHIP and Children’s Coverage, Report to Congress from the Medicaid and CHIP Payment Advisory Commission (MACPAC), March 2017, p. 7, available at https://www.macpac.gov/wp-content/uploads/2017/03/The-Future-of-CHIP-and-Childrens-Coverage.pdf.[/note] but in 2017 started going back up, rising a full percentage point between 2016 and 2019 (see…
-
Build Back Better Act: Health Coverage Provisions Explained
On November 19, 2021, the House of Representatives passed the Build Back Better Act, the budget reconciliation bill, with the Senate expected to consider the legislation in coming weeks. The Build Back Better Act includes numerous provisions that would dramatically strengthen and expand both public and private health insurance coverage. Some of the new provisions…
-
Reconciliation Bill Would Phase Out Medicaid Continuous Coverage Requirement with Key Enrollee Protections
There are many positive provisions in the Build Back Better Act (BBB) reconciliation bill as described by my colleague, Edwin Park, including filling the Medicaid coverage gap in non-expansion states, extending postpartum coverage, and making CHIP permanent. The BBB bill also phases out the 6.2 percentage point increase in the federal Medicaid funding and allows…
-
To Avoid Big Coverage Losses, Marketplaces Need to Prepare for the End of the Public Health Emergency
By Sabrina Corlette and Megan Houston The COVID-19 pandemic will end, and with it the federal government is expected to lift the “Public Health Emergency” (PHE) first declared on January 31, 2020 and extended seven times since then. Allowing the PHE to expire is more than the symbolic end of the pandemic; it signals the termination of numerous policies…
-
What’s New for 2022 Marketplace Enrollment?
Open Enrollment is just around the corner. There are new policies for the marketplace in 2022, including an expansion of opportunities to sign up for health coverage during and outside the annual open enrollment period. There are also new opportunities to get financial help with the enactment of the American Rescue Plan (ARP) Act. Here…
-
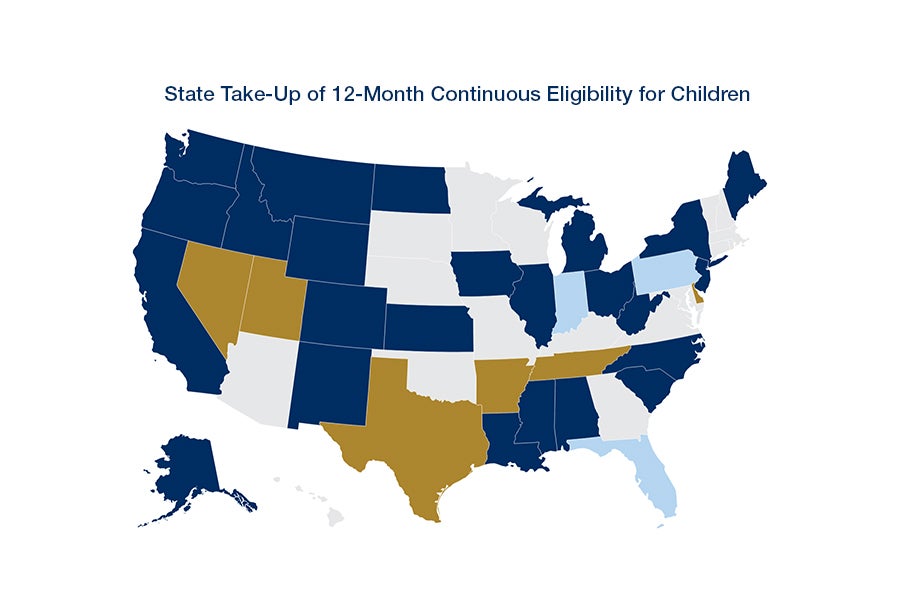
Covid-19 Exposed Many Inequities for Latino Families, Adopting Continuous Eligibility Would Repair Cracks and Protect More Latino Kids from Losing Medicaid/CHIP
COVID-19 underscores the need for universal access to health care and exposes the coverage inequities in our system today. Latino children are more likely to be uninsured than their non-Latino peers, and this coverage gap widened in recent years. A new report from CCF and UnidosUS shows that because Latino children are more likely to be…
-
Advancing Health Equity for Children and Adults with a Critical Tool: Medicaid and Children’s Health Insurance Program Continuous Coverage
Key Takeaways: Latino children disproportionately receive their health coverage through Medicaid or CHIP. Together, these programs provide coverage for more than one-third (37.6 percent) of all children, but more than half (52.1 percent) of Latino children. Adopting Medicaid and CHIP policies that remove barriers to participation and reduce gaps in coverage would narrow inequities in…
-
Medicaid Continuous Coverage Extended with Renewal of the PHE
The Biden administration has extended the public health emergency (PHE) for 90 days, from October 18, 2021 through January 16, 2022. What does this mean for Medicaid? First, the maintenance of effort provisions in the Families First Coronavirus Response Act remain in effect until January 31, 2022 (the end of the month after the PHE…
-
Why is Medicaid/CHIP Continuous Eligibility So Important for Kids?
As readers of SayAhhh! know, the number of uninsured kids was going down for many years, but during the Trump administration starting going back up – rising to 5.7 percent child uninsured rate in 2019. While children are insured at higher rates than non-elderly adults, they still lag considerably behind seniors – who with Medicare…
-
Loss of Medicaid After the PHE Will Likely Exceed 15 Million Estimated by Urban
The Urban Institute recently released a new report projecting that Medicaid and CHIP will have provided access to health care (and peace of mind) for an additional 17 million children and adults by the end of 2021. The increase is largely due to the COVID-related requirement that states keep Medicaid enrollees continuously covered during the…
-
New! Tips for Advocates on Preparing for Unwinding of the PHE Continuous Eligibility Provision
[Editor’s Note: A new version of our Tips and Best Practices for Unwinding the Medicaid Continuous Coverage Protection can be found here.] Although the end of the public health emergency (PHE) remains a moving target, it’s not too early to start planning for phasing out the continuous eligibility maintenance of effort provision and the eventual…
-
Participation of Eligible, Uninsured Children in Medicaid and CHIP Declined Again in 2019
[Editor’s Note: You can find state level Medicaid/CHIP participation rates on CCF’s State Data Hub.] Since the American Community Survey (ACS) was first released in 2008, the Urban Institute has estimated the share of uninsured children who are eligible but not enrolled in Medicaid and CHIP. Several weeks ago, Urban released its latest analysis based…
-
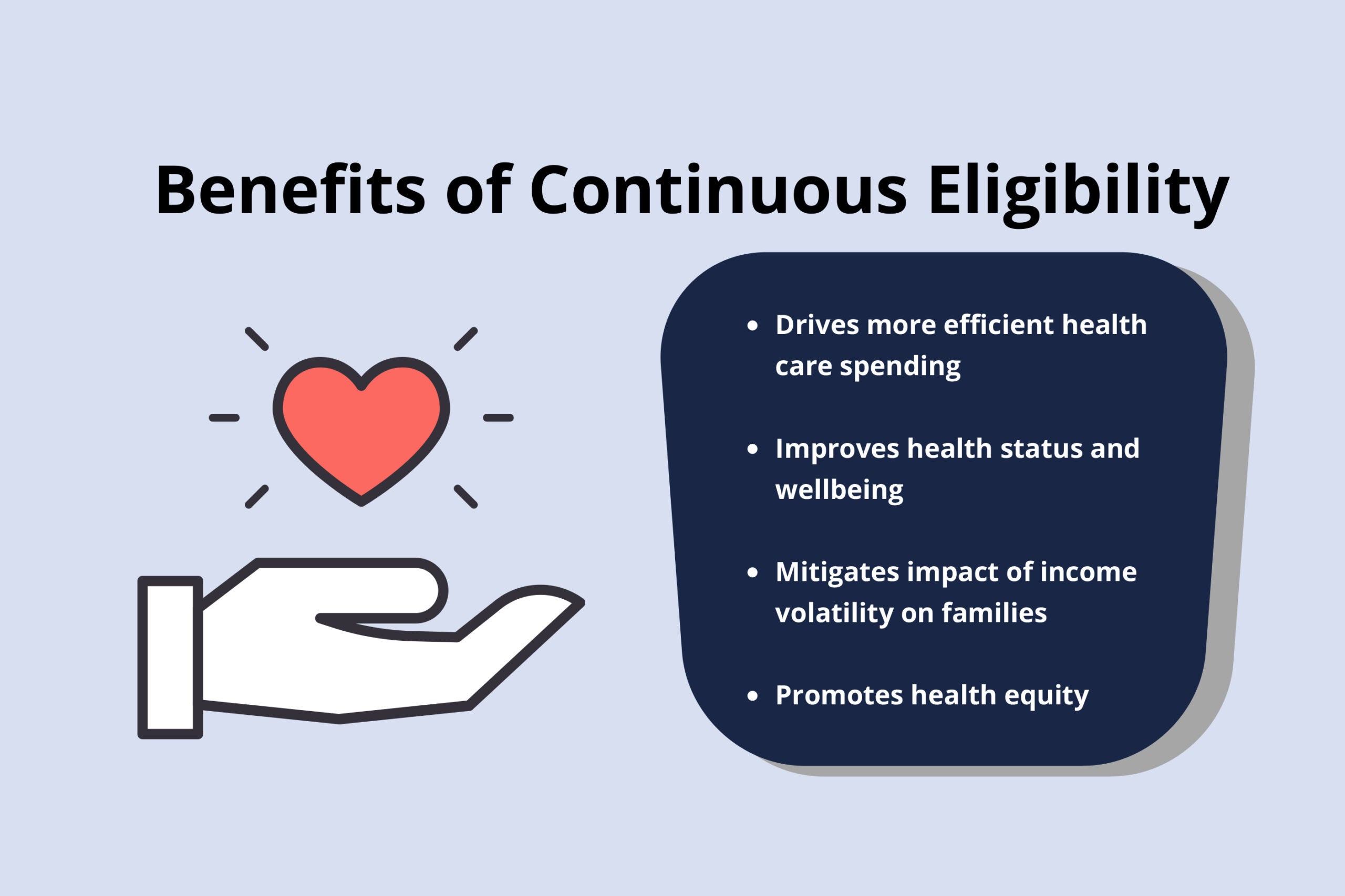
Medicaid Continuous Eligibility Linked with Better Health, More Efficient Health Care Spending
Continuous health insurance coverage produces a broad array of benefits across the health care sector for individuals, states, health plans, and providers. In particular, Medicaid continuous eligibility promotes health equity by limiting gaps in coverage for low-income children and adults who experience disproportionate rates of health disparities. Consistent access to health care, including management of…
-
Continuous Coverage in Medicaid and CHIP
Executive Summary Continuous health insurance coverage produces a broad array of benefits across the health care sector for individuals, states, health plans, and providers. In particular, Medicaid continuous eligibility promotes health equity by limiting gaps in coverage for low-income children and adults who experience disproportionate rates of health disparities. Consistent access to health care, including…
-
Opportunities to Improve Guidance on Phasing out the Public Health Emergency Continuous Eligibility Provision
In December 2020, the Trump administration issued guidance on unwinding the Medicaid continuous eligibility provision associated with the COVID-19 public health emergency (PHE). There are a number of opportunities for the Biden administration or Congress to strengthen requirements for states to ensure that eligible Medicaid enrollees do not lose coverage at the end of the…
-
States Move Toward Multi-Year Continuous Eligibility for Children in Medicaid
Children need consistent access to health care, especially in their early years when frequent screenings, vaccinations, and well child checkups are so critical to their development and school readiness. And despite efforts to streamline and simplify eligibility processes and improve retention, many children covered by Medicaid (as well as other sources of health insurance) experience…
-
Kaiser Family Foundation and Georgetown CCF Release 50-State Survey on Medicaid and CHIP Eligibility and Enrollment
The 2021 Annual 50-State Survey on Medicaid and CHIP Eligibility and Enrollment conducted by the Kaiser Family Foundation (KFF) and CCF is now available. As in previous years, the report confirms eligibility levels for children, pregnant women, parents and expansion adults. However, in light of the ongoing COVID-19 pandemic, the survey was scaled back in…